
The above painting shows glomeruli with nodular mesangial expansion and arterial hyalinosis, changes frequently seen in diabetic nephropathy. Diabetic nephropathy is graded by the classification system established by the Renal Pathology Society to separate lesions into varying degrees of severity. In class I diabetic glomerulopathy, there are no changes identified by light microscopy, but thickening of the glomerular basement membranes are seen on electron microscopy (see photomicrograph below). Thickened glomerular basement membranes are greater than 471 nm in women or 520 nm in men (in our lab), which represents greater than 2 standard deviations above the normal population. Glomerular basement membrane thickening is the earliest change in diabetic nephropathy, and can increase with disease duration and progression. In class II diabetic glomerulopathy, there is mild (class II A) or severe (class II B) mesangial expansion within glomeruli. In class III, there is nodular diabetic glomerulosclerosis, with formation of at least one Kimmelstiel-Wilson nodule (see photomicrograph below). In class IV disease, there is advanced diabetic glomerulosclerosis with greater than 50% global glomerulosclerosis (Tervaert TWC et al, 2010). A diabetes classification is included within renal biopsy reports to provide a degree of severity of the patient’s diabetic nephropathy, as well as for comparison in patients who may have a repeat biopsy in the future. It should not be used to inform prognosis in diabetic nephropathy.
Diabetic nephropathy carries a heavy disease burden, affecting 30-40 percent of patients with diabetes mellitus, and is a major cause of end-stage kidney disease in these patients. Since all patients with diabetes mellitus do not all develop diabetic kidney disease and progression of kidney disease varies among individuals, studies are ongoing to identify genetic and environmental factors that place patients at risk. This is the basis of TRIDENT (Transformative Research In Diabetic Nephropathy), an ongoing prospective observational cohort study utilizing genetic and biomarker testing (clinicaltrials.gov identifier: NCT0298684).
Diabetic nephropathy has been treated with tight glucose control and anti-proteinuric therapy with renin-angiotensin system blockade. While this can delay progression, it still occurs with worsening chronic kidney disease or end stage kidney disease in many patients. A recent study, Canagliflozin, and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE), established a benefit for use of sodium-glucose cotransporter-2 (SGLT2) inhibitors in diabetic nephropathy. The SGLT2 inhibitor canagliflozin was found to reduce progression of diabetic nephropathy as well as reduce cardiovascular events (Perkovic V et al, 2019).
SGLT2 inhibitors reduce serum glucose levels (leading to a marginally reduced hemoglobin A1c), reduce blood pressure, and promote weight loss by increasing glycosuria at the proximal tubule. This reduces the solute load to the macula densa, which results in less release of ATP from the basolateral membrane of tubular epithelial cells. This in turn, reduces adenosine production, causing less activation of the A1 receptor and prevents vasodilation at the afferent arterioles. In a mouse model of overflow proteinuria by excessive administration of bovine serum albumin, treatment with an SGLT2 inhibitor reduced proteinuria by preservation of the podocyte cytoskeleton (Cassis P et al, 2018). Therefore, SGLT2 inhibition may also be protective to podocytes, which could reduce proteinuria through maintenance of podocyte foot processes.
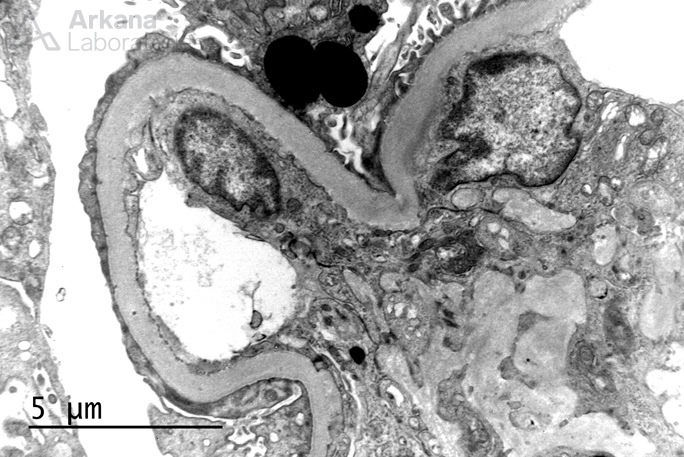
Thickened glomerular basement membranes.
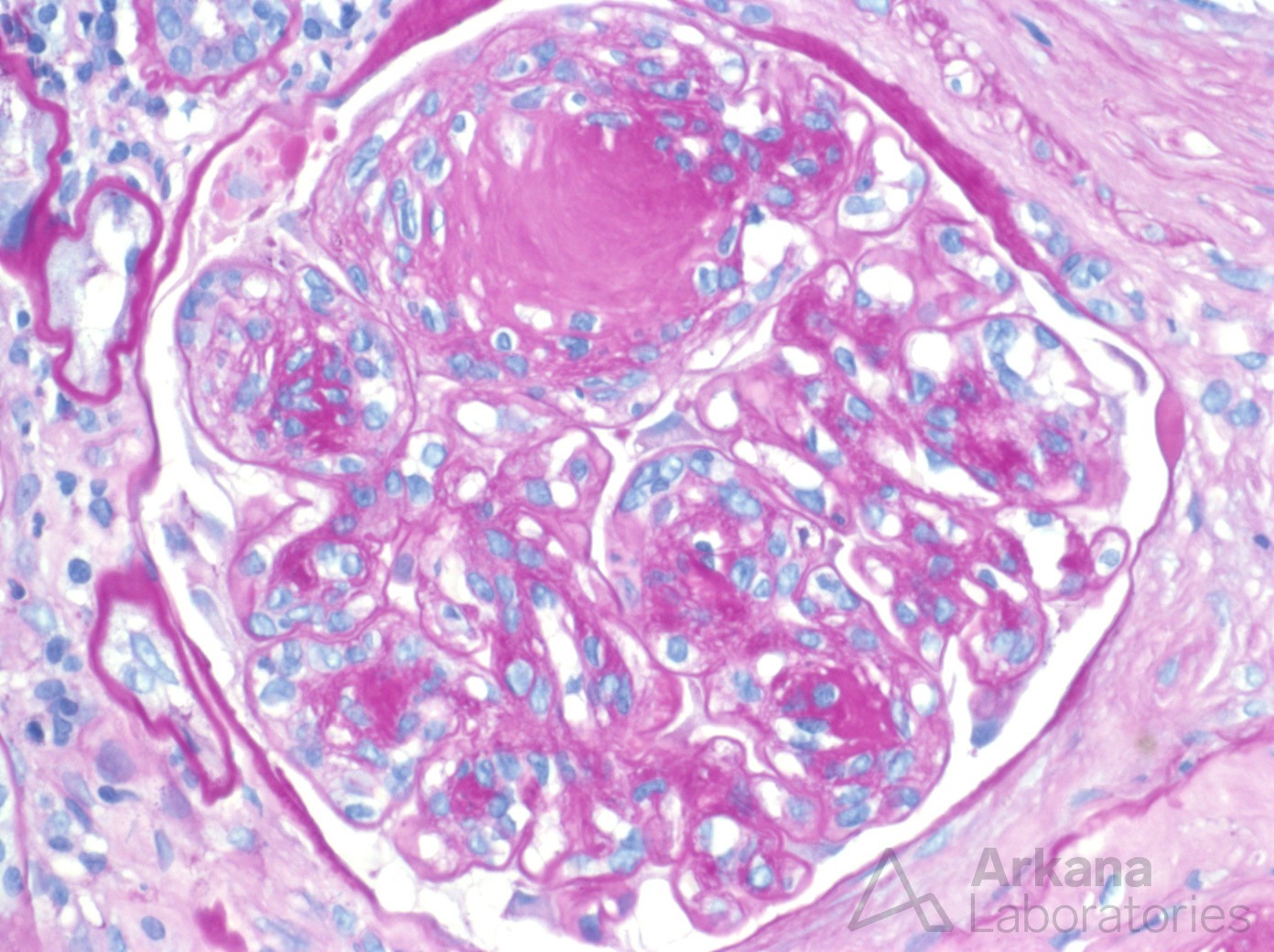
Nodular diabetic glomerulosclerosis.
References:
Cassis P, Locatelli M, Cerullo D, Carna D, Buelli S, Zanchi C, Villa S, Morigi M, Remuzzi G, Benigni A, Zoja C. SGLT2 inhibitor dapagliflozin limits podocyte damage in proteinuric diabetic nephropathy. JCI Insight 2018 Aug 9; 3 (15): pii98720.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu PL, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H, Zinman B, Meininger G, Brenner BM, Mahaffey KW; CREDENCE Trial Investigators. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. New England Journal of Medicine April 14.
Tervaert TWC, Mooyaart AL, Amann K, Cohen AH, Cook HT, Dachenberg CB, Ferrano F, Fogo AB, Haas M, de Heer E, Joh K, Noel LH, Radhakrishnan J, Seshan SV, Bajema IM, Bruijn JA, and the Renal Pathology Society. Pathologic Classification of Diabetic Nephropathy. J Am Soc Nephrol 2010; 21 (4): 556-563.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.

