Clinical History:
This 69-year-old patient presents with bilateral leg weakness and falls. Past medical history includes lumbosacral spinal stenosis, hypertension, and type II diabetes. Medications include glipizide and atorvastatin which was stopped one year prior, and MRI of cervical is C6-C7 stenosis. Patient’s lab results was CK 960 u/L, and HMGCR antibody positive.
Question:
What is the most likely diagnosis?
A. Immune mediated necrotizing myopathy
B. Dermatomyositis
C. Toxic Myopathy
D. Mitochondrial myopathy
Answer: A. Immune mediated necrotizing myopathy
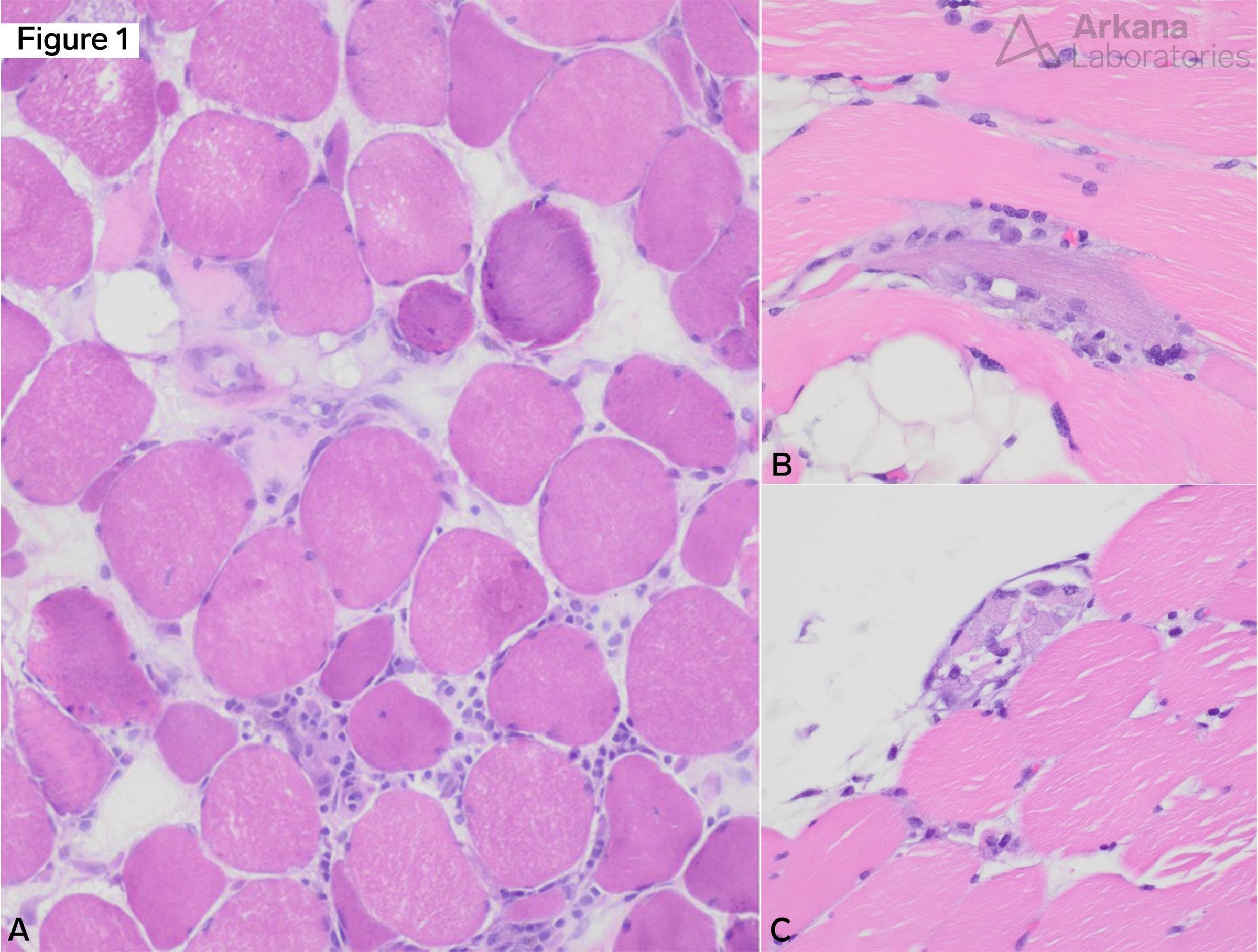
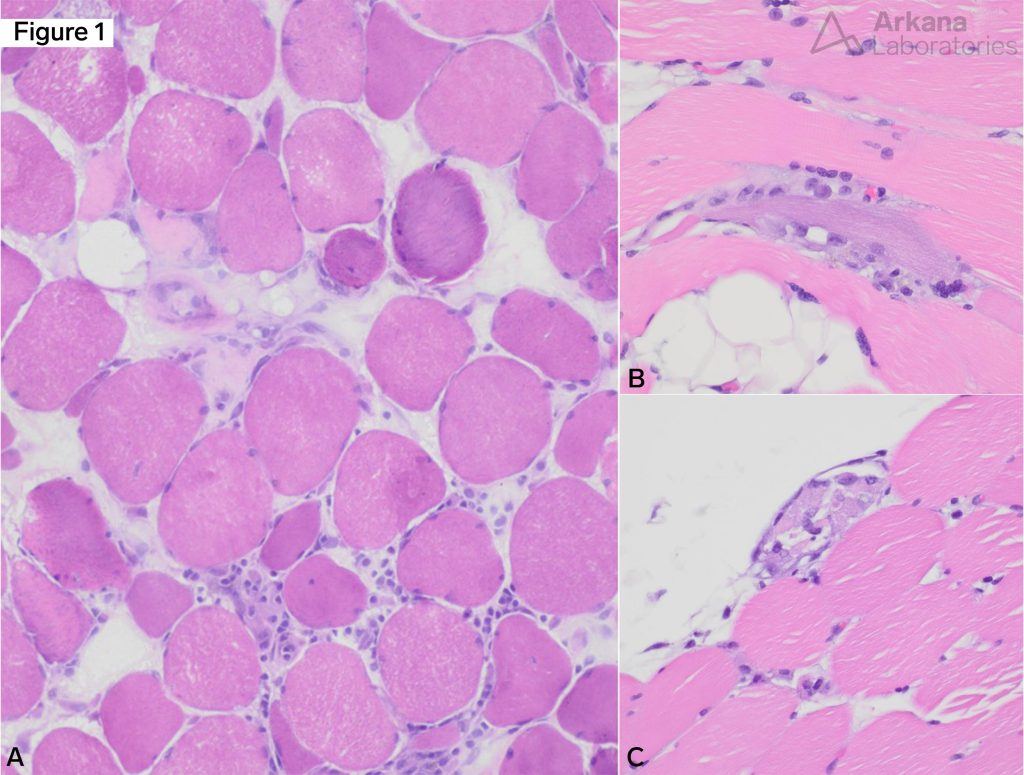
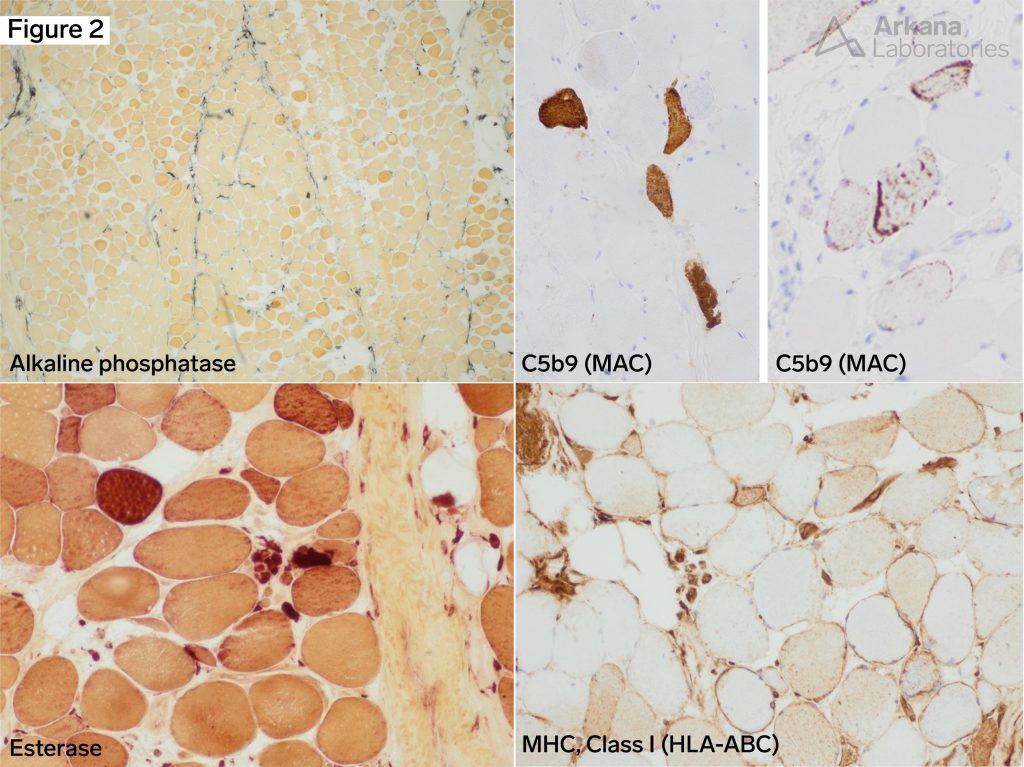
- Positive HMGCR (or SRP) serology combined with scattered necrotic fibers without significant lymphocytic inflammation are characteristic.
- Perifascicular alkaline phosphatase staining is seen in both dermatomyositis (DM) and IMNM. In this case, other DM-associated pathology (perifascicular atrophy, necrosis and inflammation) are not seen. HMGCR antibodies are also not associated with DM.
- A direct, toxic, stain-induced myopathy is also possible, but continued necrosis 12 months later is less common. Statin use is a common precipitating factor in IMNM.
- The ragged red fibers and SDH positive/COX negative fibers characteristic of a mitochondrial myopathy are not present.
Necrotizing Myopathy
IMNM is only one possible etiology of necrotic fibers without significant inflammation. Other etiologies include:
- Partially treated acquired inflammatory myopathy
- Paraneoplastic myopathy
- Metabolic myopathy
- Endocrine myopathy
- Viral myopathy
Reference(s)/additional reading:
Uruha A, Goebel HH, Stenzel W. Updates on the Immunopathology in Idiopathic Inflammatory Myopathies. Curr Rheumatol Rep. 2021; 23:56.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.