This biopsy came to us for a workup on proteinuria.
The patient is a 68-year-old female with a history of “low-grade non-Hodgkin’s lymphoma” initially diagnosed in 2007. She was treated with rituximab, from November 2007 to July 2009. She was treated with Treanda (bendamustine ) during the spring of 2010. In 2010, she presented with proteinuria and a renal biopsy established the diagnosis of membranoproliferative glomerulonephritis (MPGN). Her symptoms resolved with chemotherapy and lymphoma treatment and remission.
She now presents once again with proteinuria. The patient is in remission from the lymphoma. A renal biopsy was performed to establish the cause of the proteinuria.
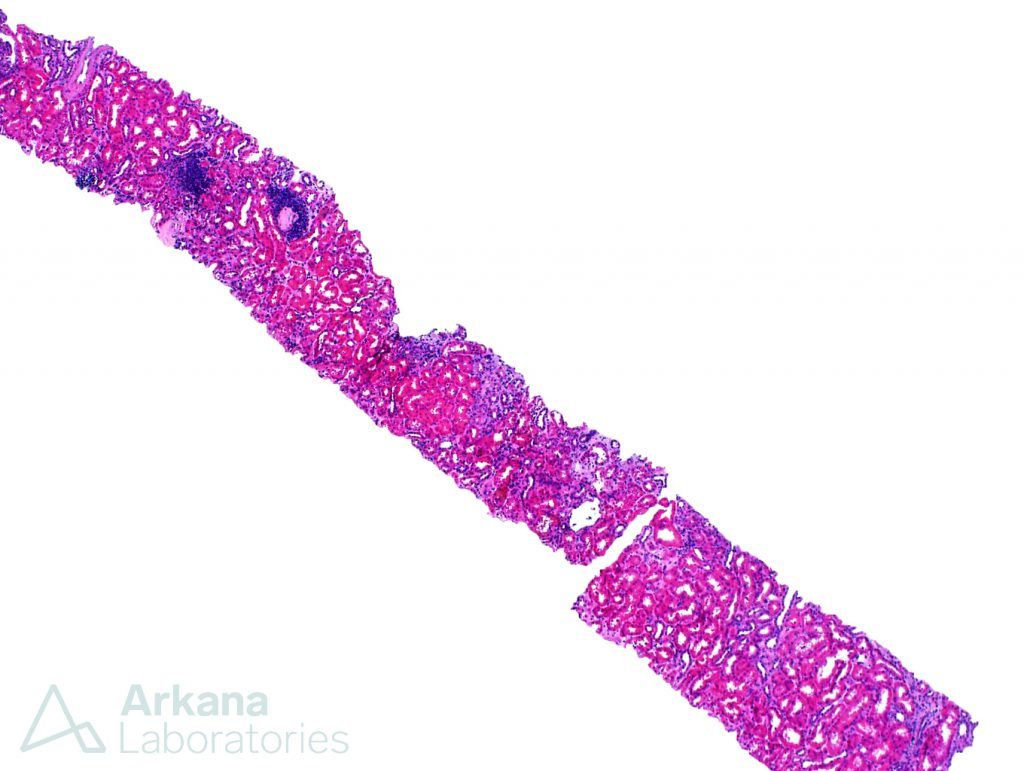
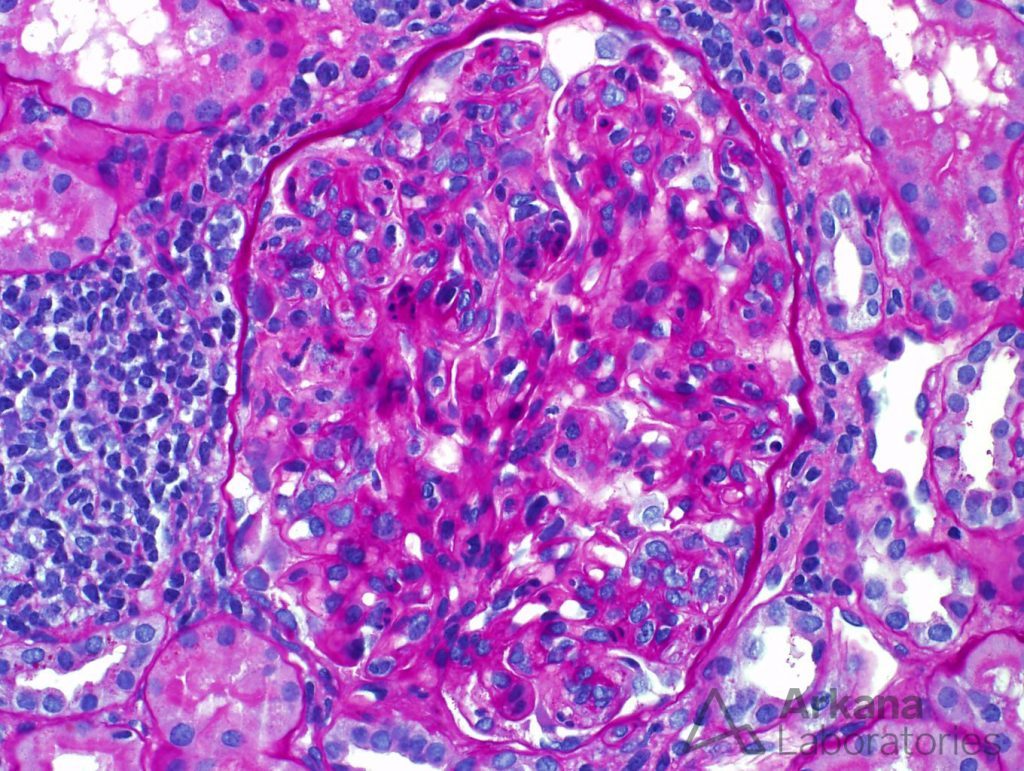
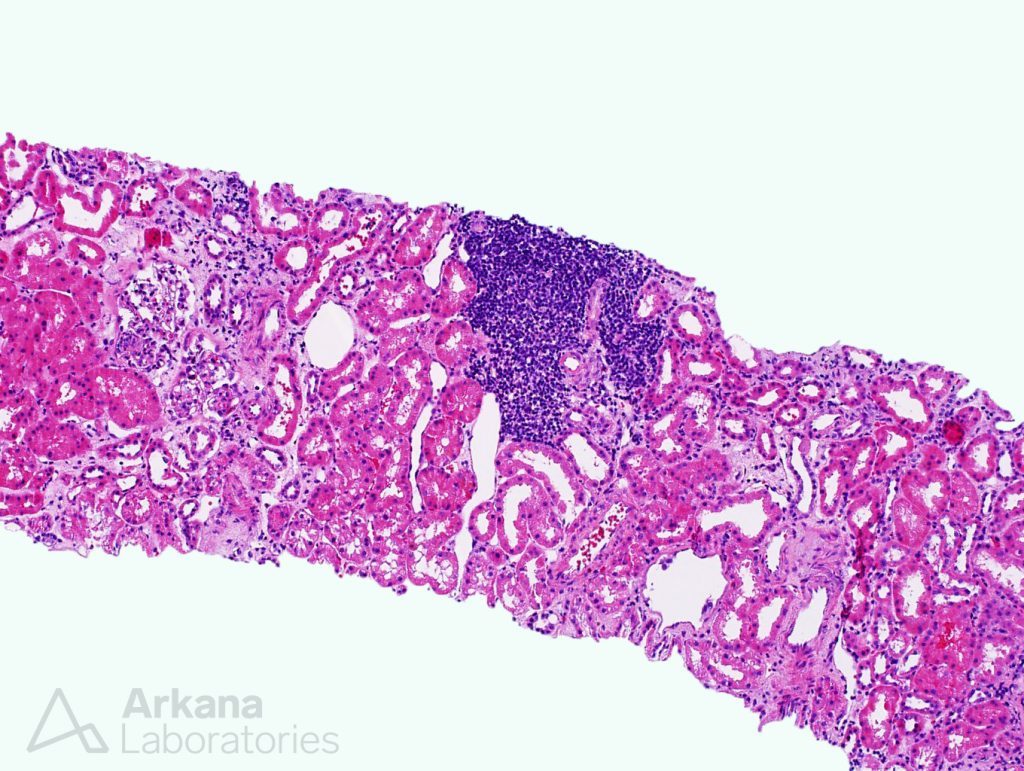
The biopsy showed a proliferative glomerulonephritis, with MPGN features, very similar to the previous presentation. Mesangial and endocapillary hypercellularity was observed in the glomeruli, and double contours were occasionally seen along capillary loops.
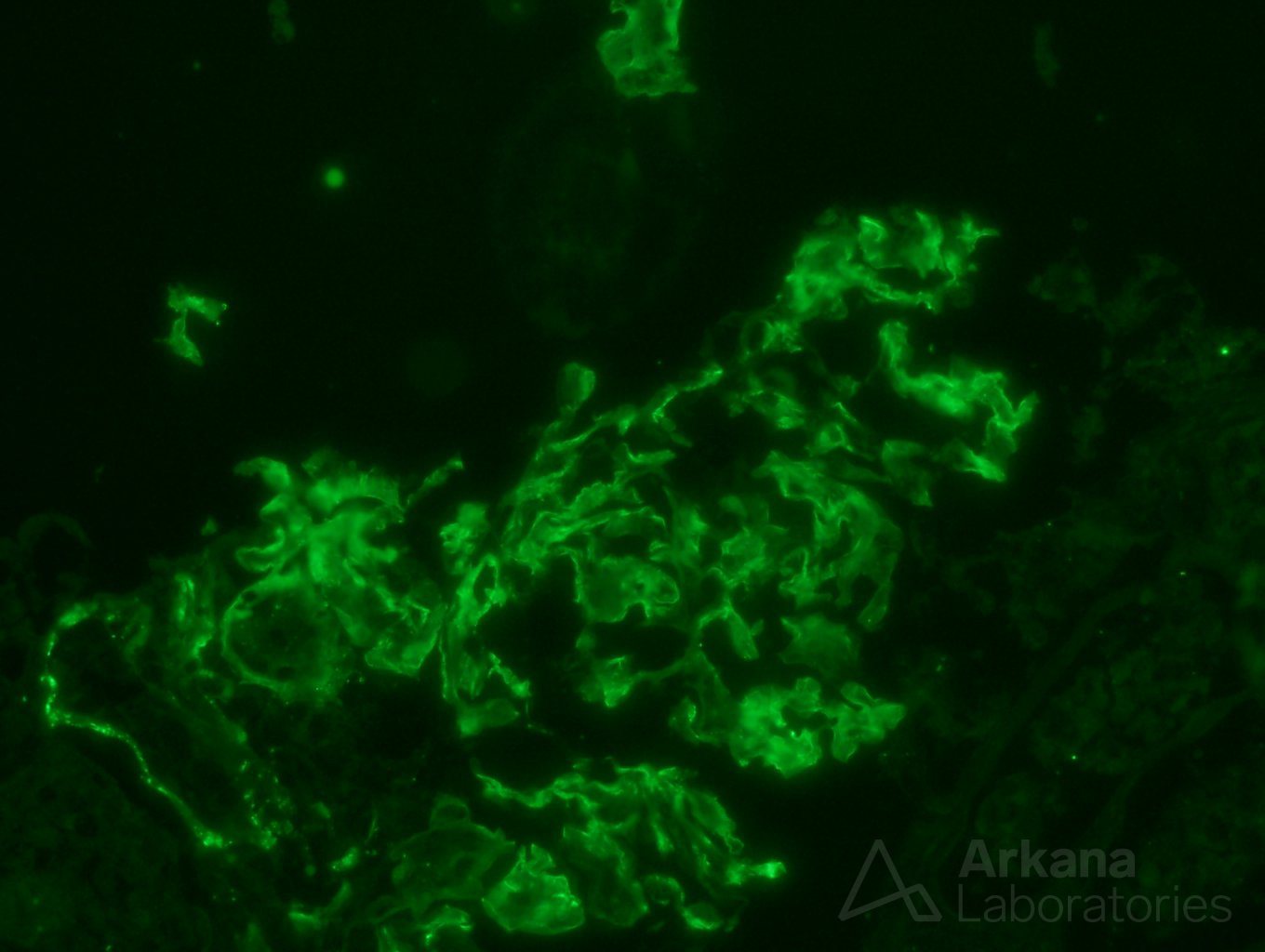
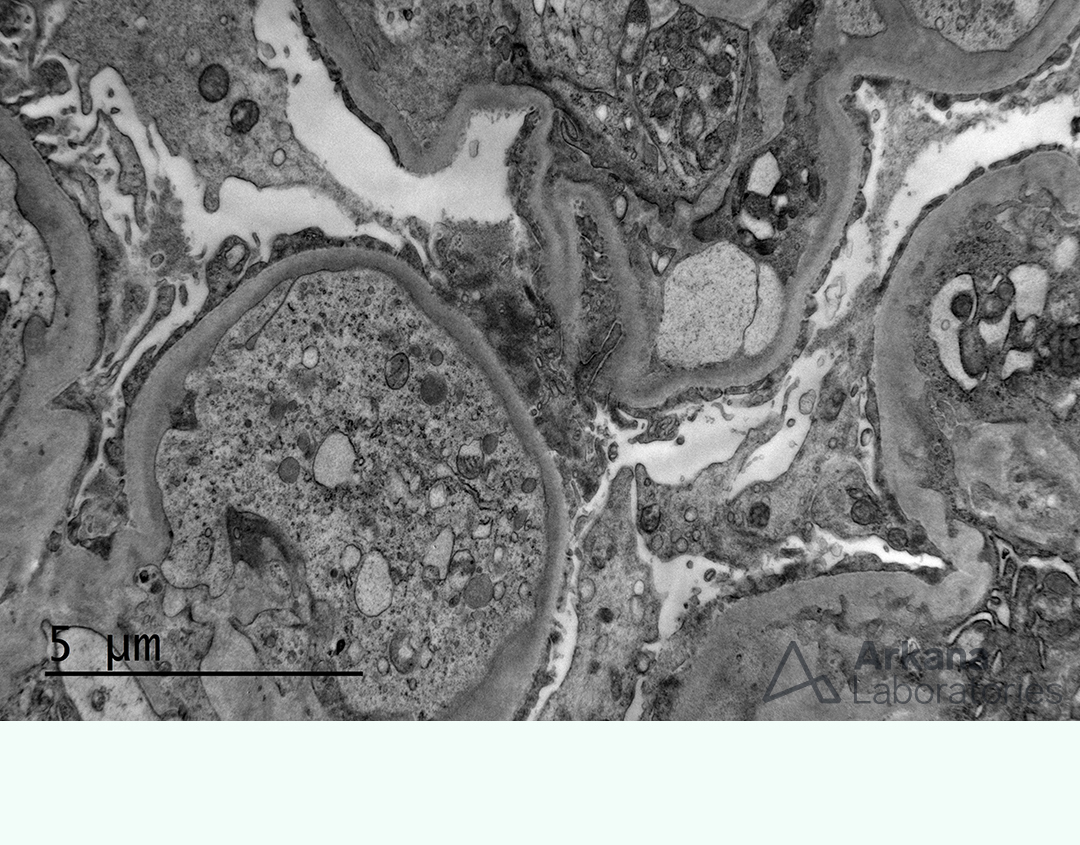
Immunofluorescence stains and electron microscopy confirmed the presence of subendothelial deposits, consistent with MPGN pattern.
At this point, a diagnosis of membranoproliferative glomerulonephritis (MPGN) had been established, and fully explained the patient’s proteinuria.
However, another finding in the biopsy was the presence of interstitial LYMPHOID AGGREGATES, which had an inconspicuous, if not innocent, appearance.
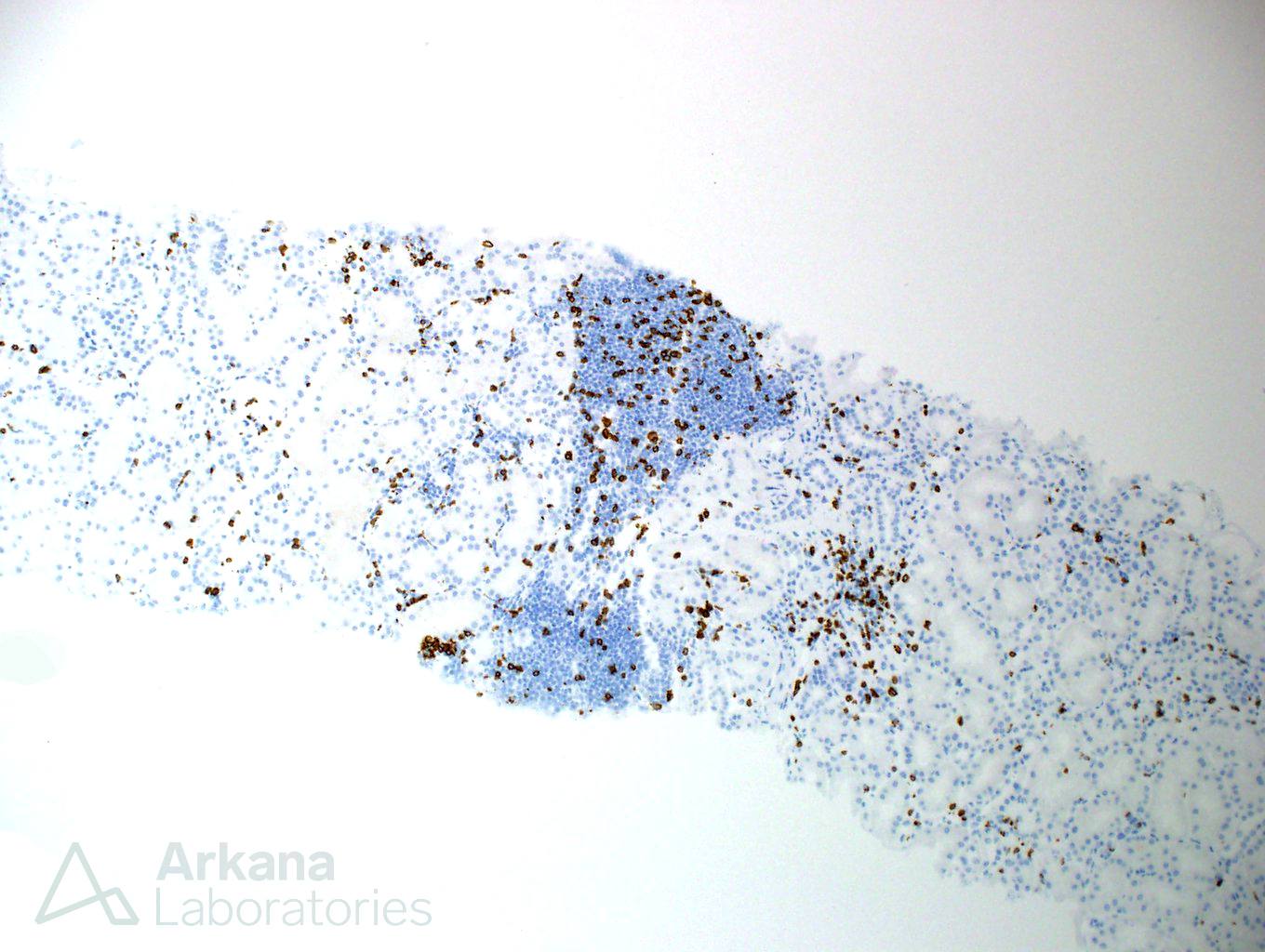
Unsettled with the history of lymphoma, and observing that the patient had a similar clinical presentation and histologic features in the past, we decided to dig deeper and ordered CD3 and CD20 immunostains to evaluate the infiltrate.
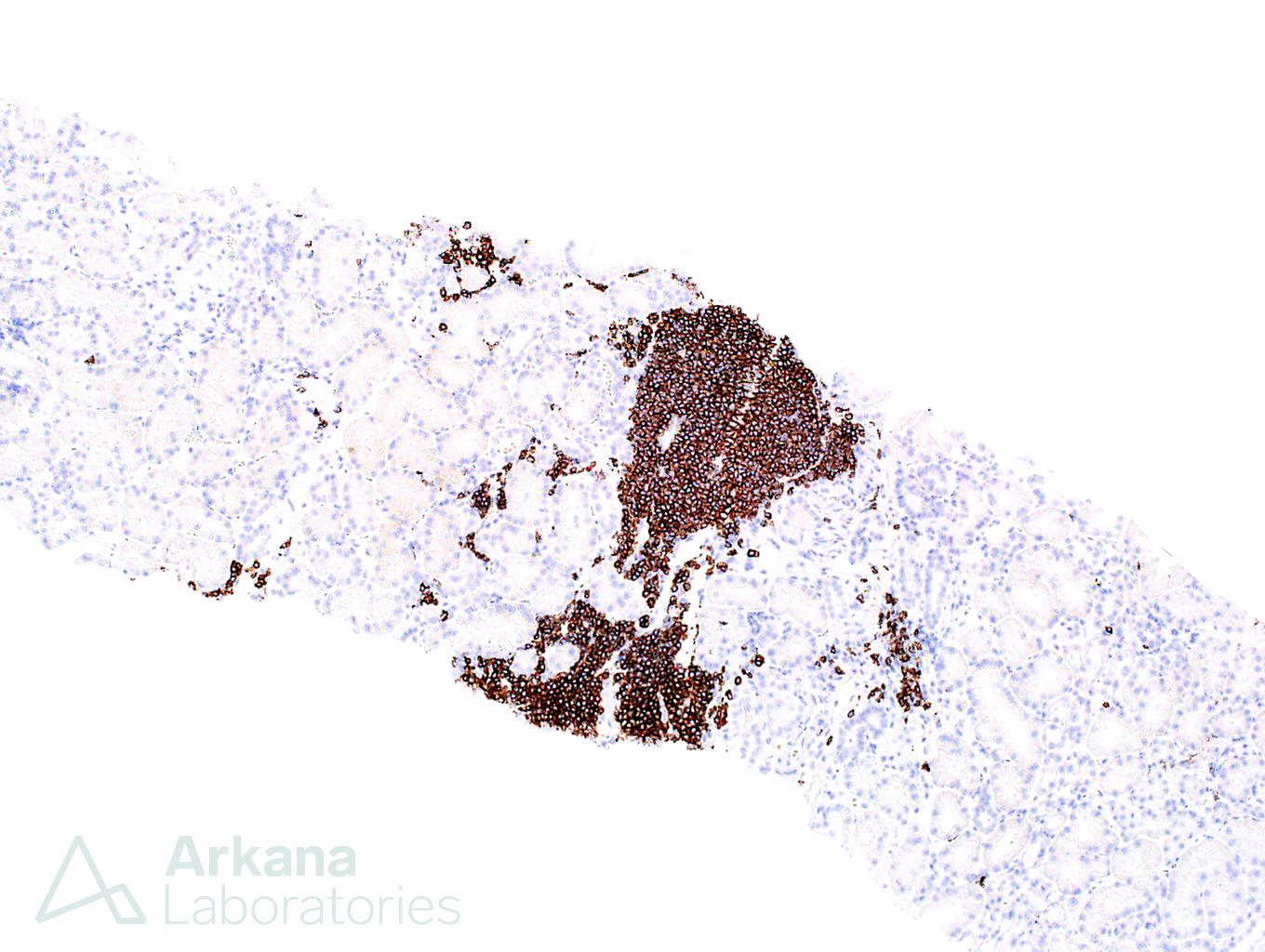
CD3 and CD20 immunostains showed that most lymphocytes had a CD20 positive phenotype – B cells. This is the opposite of what one would expect in a reactive infiltrate and is highly suspicious for lymphoma
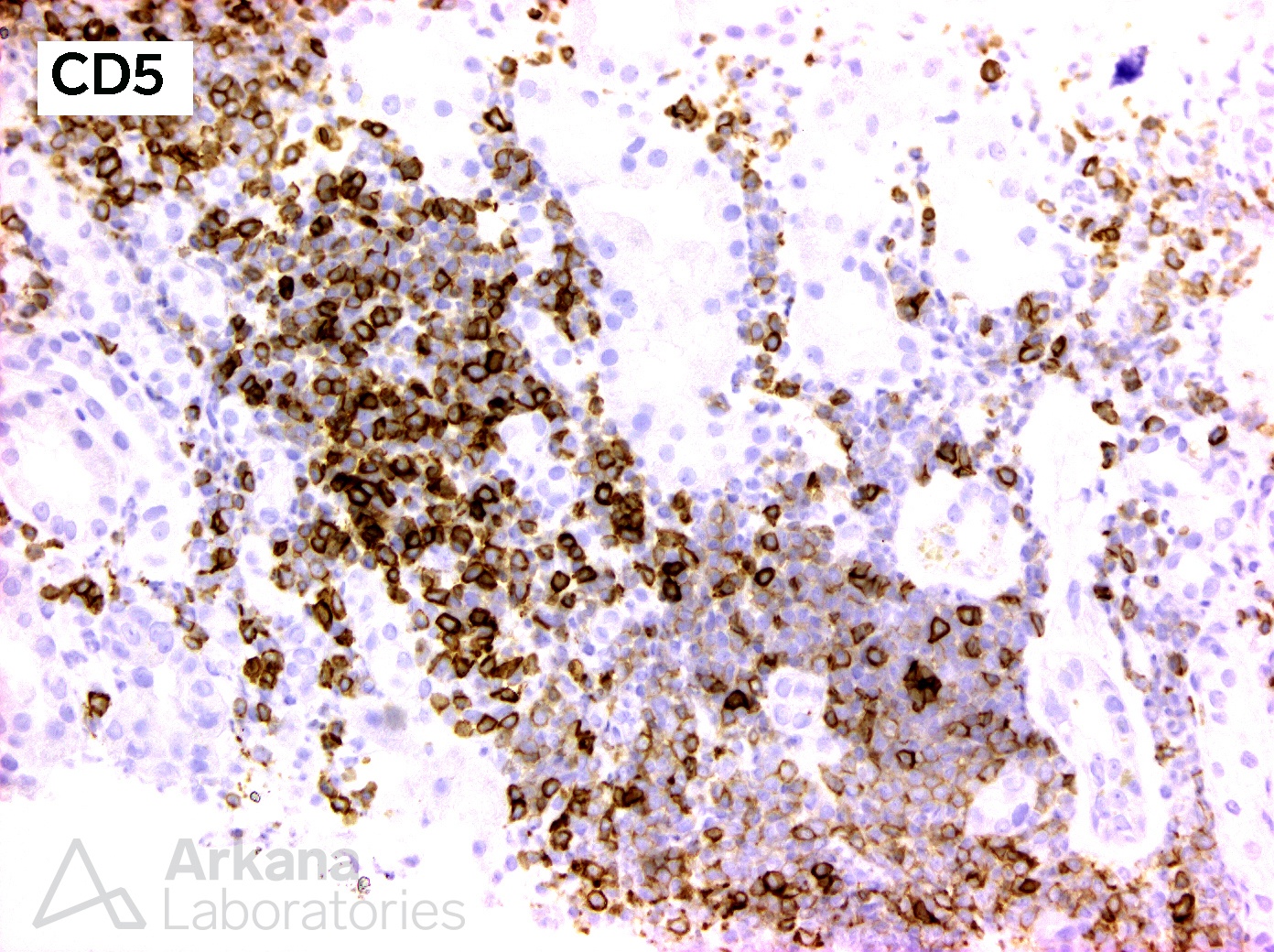
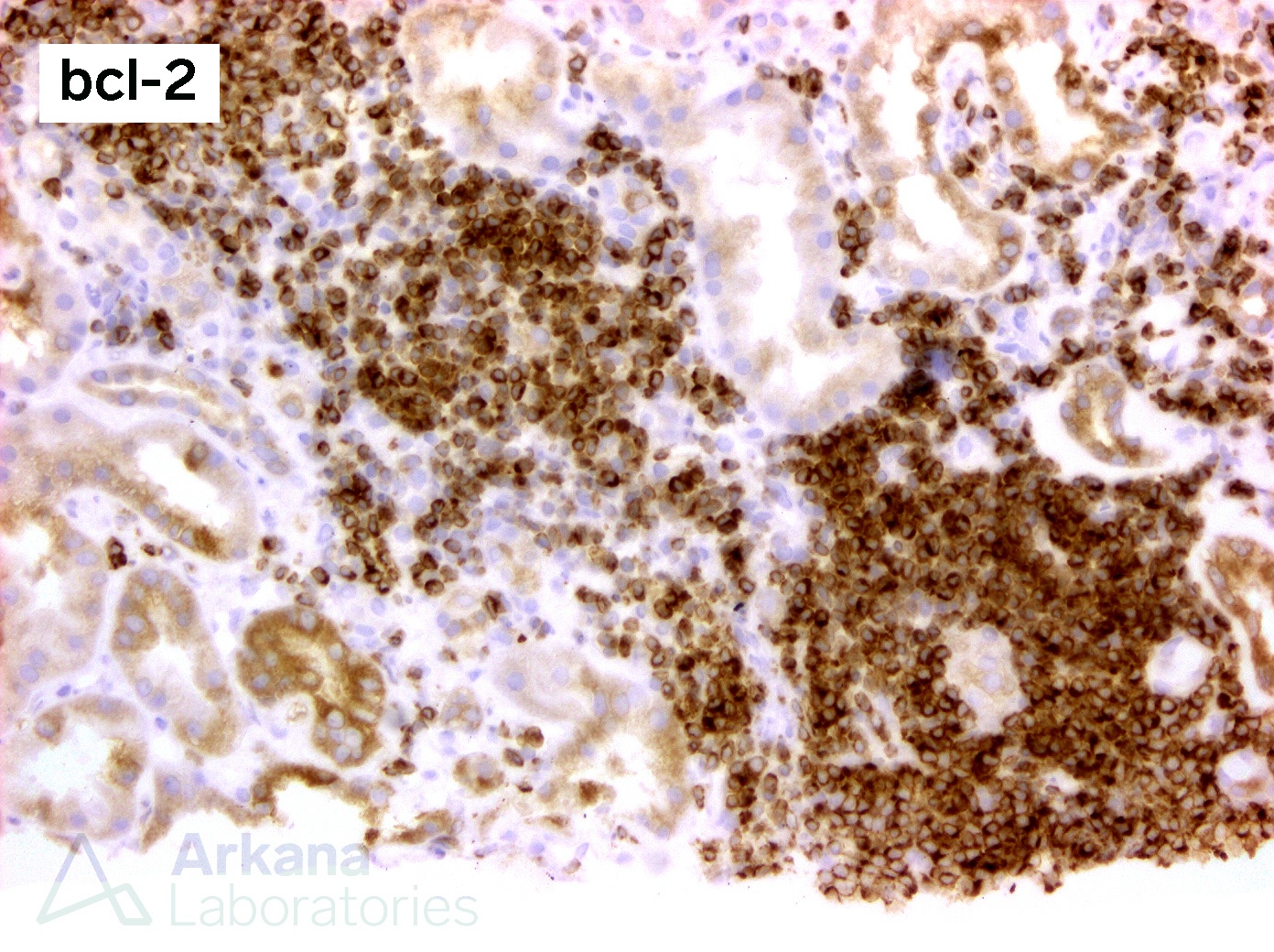
Further workup was performed, and the lymphoid cells were proven to be CD5 and bcl-2 positive (figures below), while negative for CD10 and cyclin D1. These results showed that the infiltrate was indeed consistent with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
By digging deeper into this case, we were able to prove that the patient has residual/recurrent lymphoma and that it is likely related to the recurrence of proteinuria and membranoproliferative glomerulonephritis.y related to the recurrence of proteinuria and membranoproliferative glomerulonephritis.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.