This biopsy was from a 57-year-old African American female patient. She presented with a gradual increase in serum creatinine over the course of 5 months. Initially, her baseline serum creatinine was 1.3 mg/dl but two months later it increased to 2.0 mg/dl. And, at the time of the biopsy, an additional 3 months later, her serum creatinine was as high as 4.4 mg/dl. During her workup, she was found to have nephrotic syndrome with proteinuria quantified at 8 gm/24hr, a serum albumin of 1.3 g/dL, and ascites.
Concerning previous medical history, the patient had a diagnosis of stage II colon cancer in the year prior to the biopsy and had been treated with partial colectomy and chemotherapy. She also had a history of alcohol dependence, in remission.
Serologies for ANA, rheumatoid factor, anti-dsDNA, c-ANCA, p-ANCA, hepatitis B, and hepatitis C were negative. SPEP and UPEP showed no paraprotein. C3 and C4 levels were normal.
Clinically, the physician was concerned for a glomerulonephritis, in particular, membranous glomerulopathy. This was a very reasonable hypothesis, as the patient had nephrotic syndrome, and membranous glomerulopathy has been associated with malignancy. Thus, a renal biopsy was performed to examine this possibility.
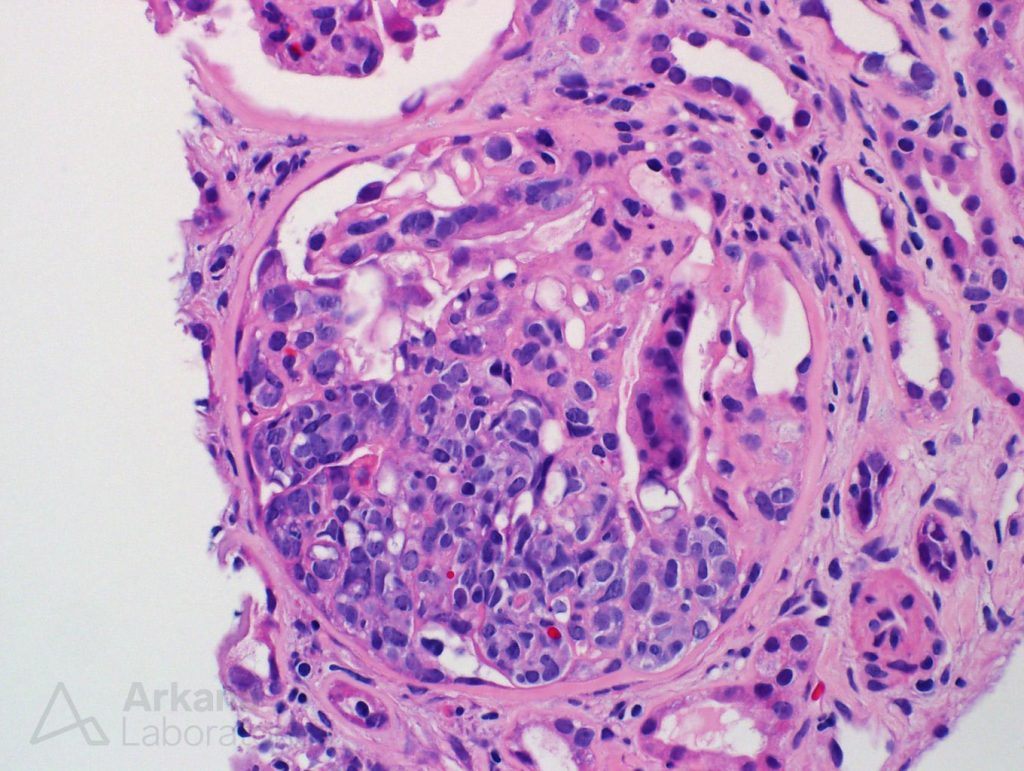
The renal biopsy contained up to sixteen glomeruli. And, the physician was correct in that the glomeruli did show injury. However, they did not have typical features of a glomerulonephritis, much less of a membranous nephropathy.
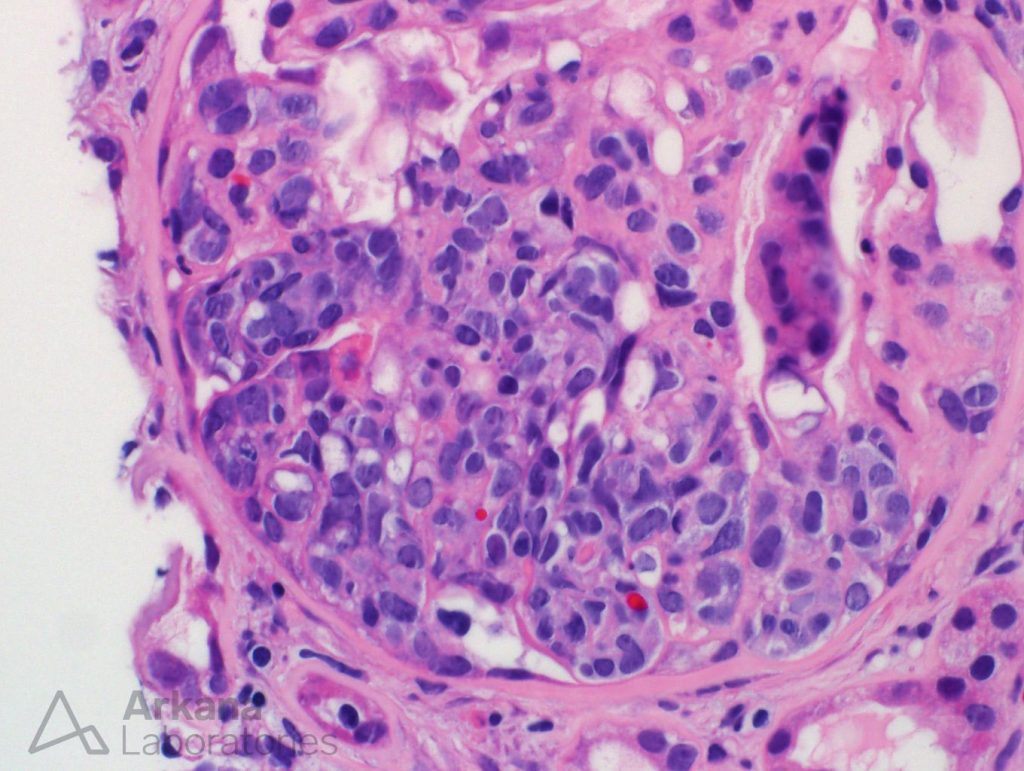
Surprisingly, the majority of the glomeruli had markedly atypical cells segmentally filling the capillary lumens. These cells looked much worse than your run-of-the-mill inflammatory cells of glomerulonephritis. These atypical cells had a high nuclear-to-cytoplasmic ratio, expanded the capillary lumen and formed loose clusters. Some of the cells look like “signet-ring cells”. In short, these atypical cells looked like CANCER cells.
Now, we will jump from Medicine to philosophy, and refer to Ockham to help us solve this case. William of Ockham (c. 1287–1347), was an English Franciscan friar, philosopher, and theologian. He developed the problem-solving principle of the “law of parsimony“, known as Ockham’s razor (also Occam’s razor; Latin: lex parsimoniae). His principle states that among competing hypotheses, the one with the fewest assumptions should be selected. In other words: the simpler, the better. And where does that leave us? Well, in a patient with a previous history of colon cancer, that has cancerous-appearing cells in the glomeruli, where are these cells coming from, Mr. Ockham? Of course, they must be from the colon!
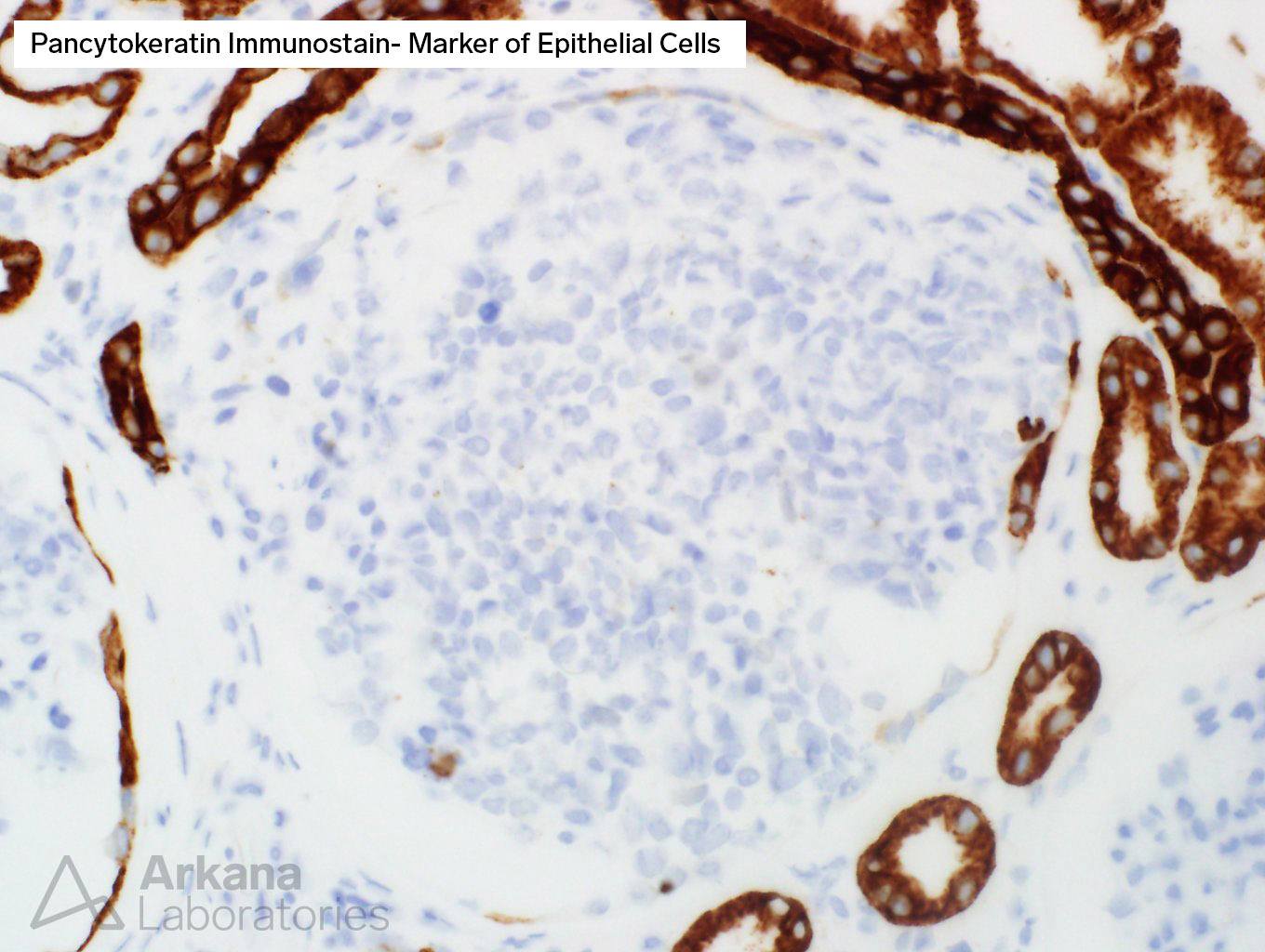
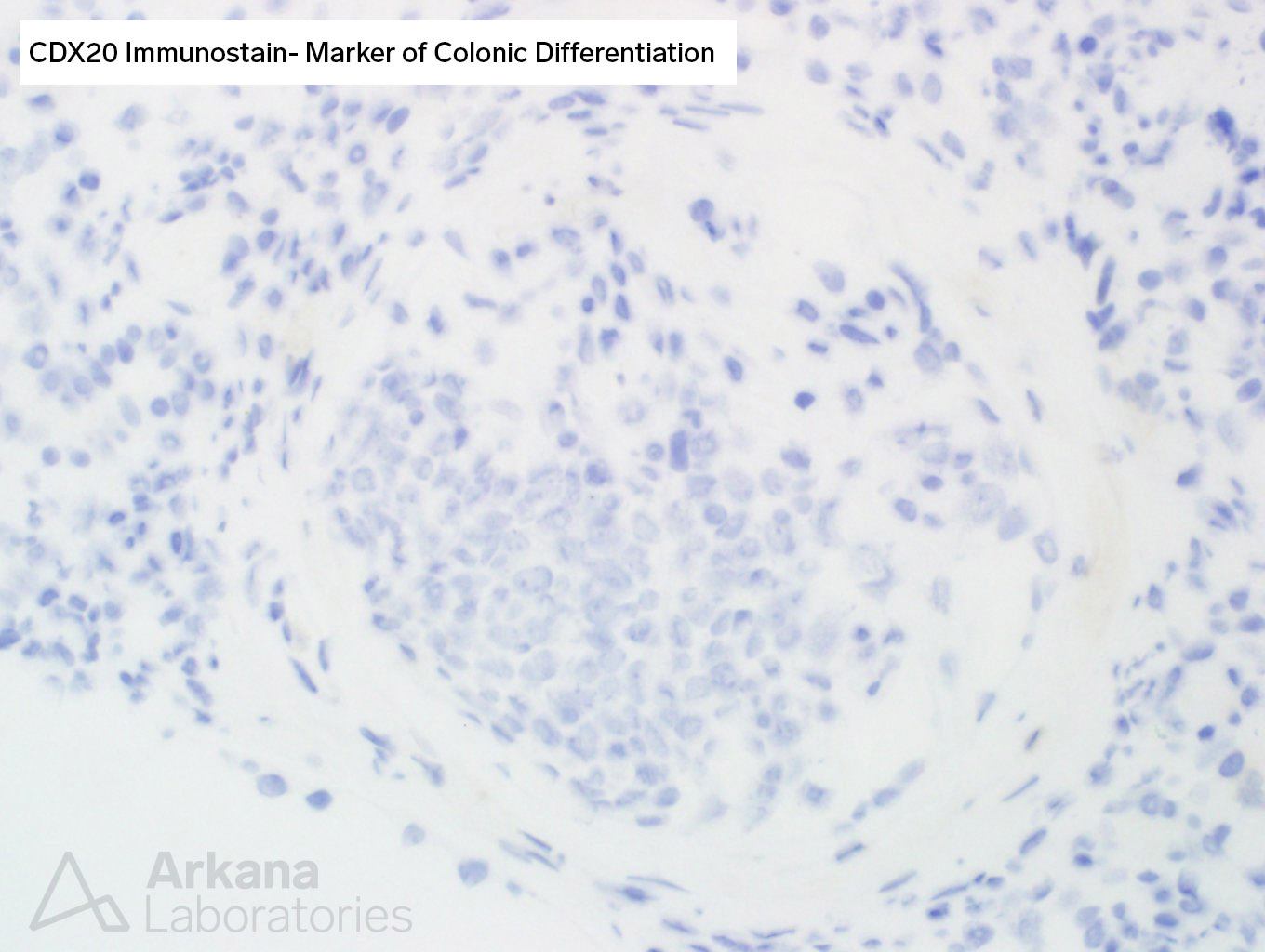
Armed with such logic, using our razor and reason, we decided to shave away any other unnecessary assumptions and tried to prove that the cells were indeed colonic cancer cells that decided to find a new home in the glomerular capillary loops. After all, cancer can do whatever it pleases, and such cases (although rare) have been described before. Thus, we ordered two stains to prove our hypothesis: pan-cytokeratin, a stain that generally stains most forms of carcinoma, and CDX2, a stain most commonly seen in colon cancer.
Too bad that our cells did not cooperate and our opinion was blasted by the fact that both stains were negative in the cancerous-appearing cells. One can clearly note how the tubular cells in the tissue stain with pancytokeratin, while the tumoral cells refuse to stain at all (picture 3).
So, what do we do now that things have taken an unexpected turn? Well, start over, dig deeper, and don’t give up.
A new set of stains was performed. This time, we tried to rule out the two other most common diagnostic possibilities for undifferentiated tumors that are not carcinoma. Our next culprits were lymphoma and melanoma.
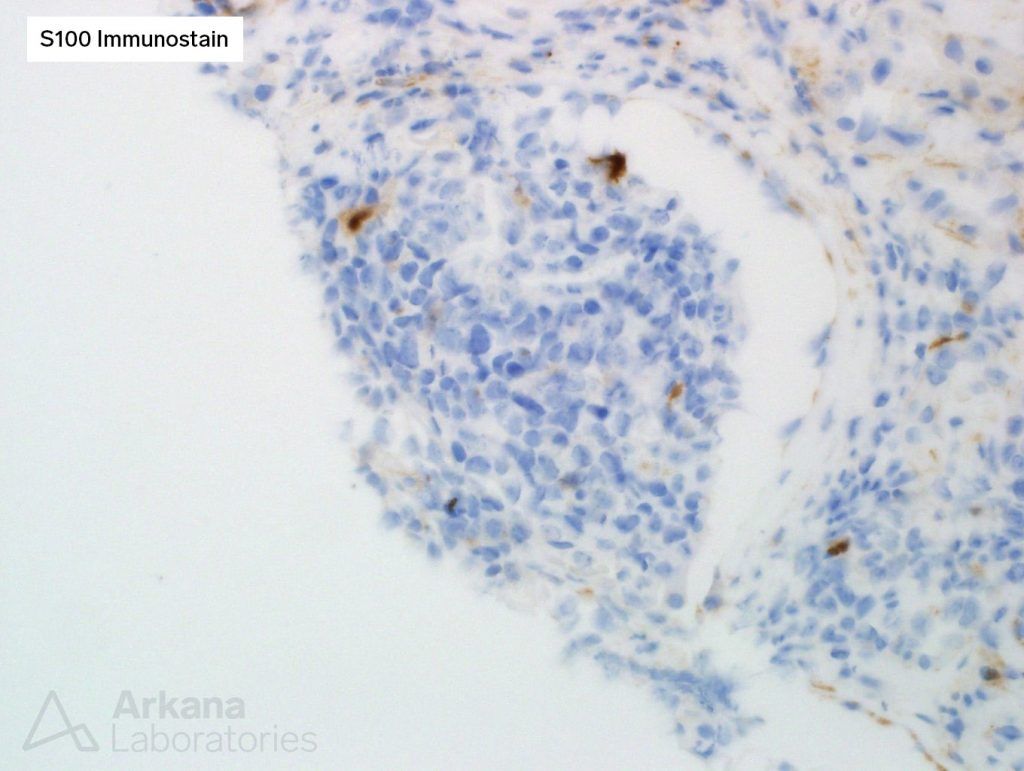
To investigate the possibility of melanoma, an S100 immunostain was performed, and it was negative in the tumor cells.
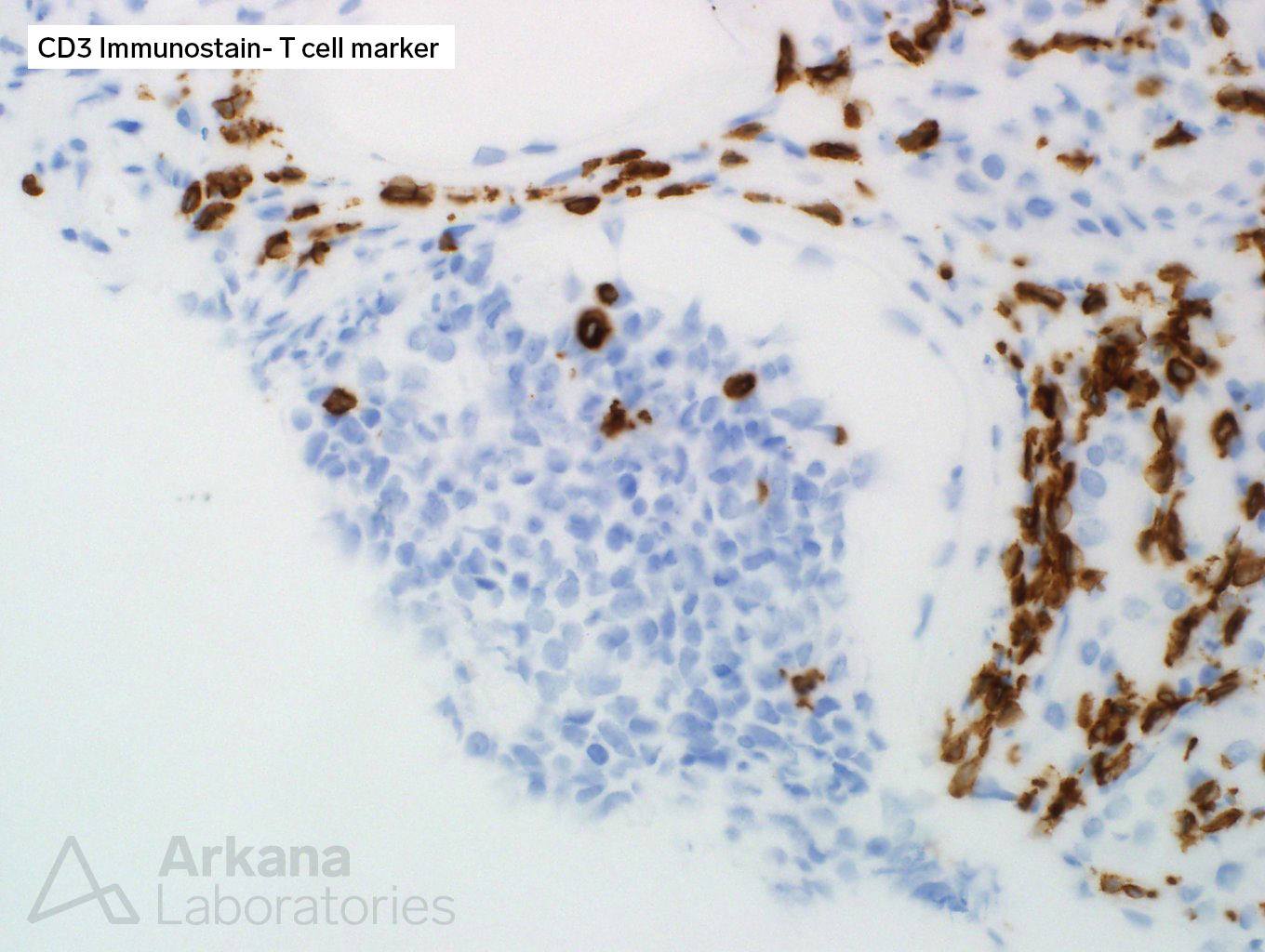
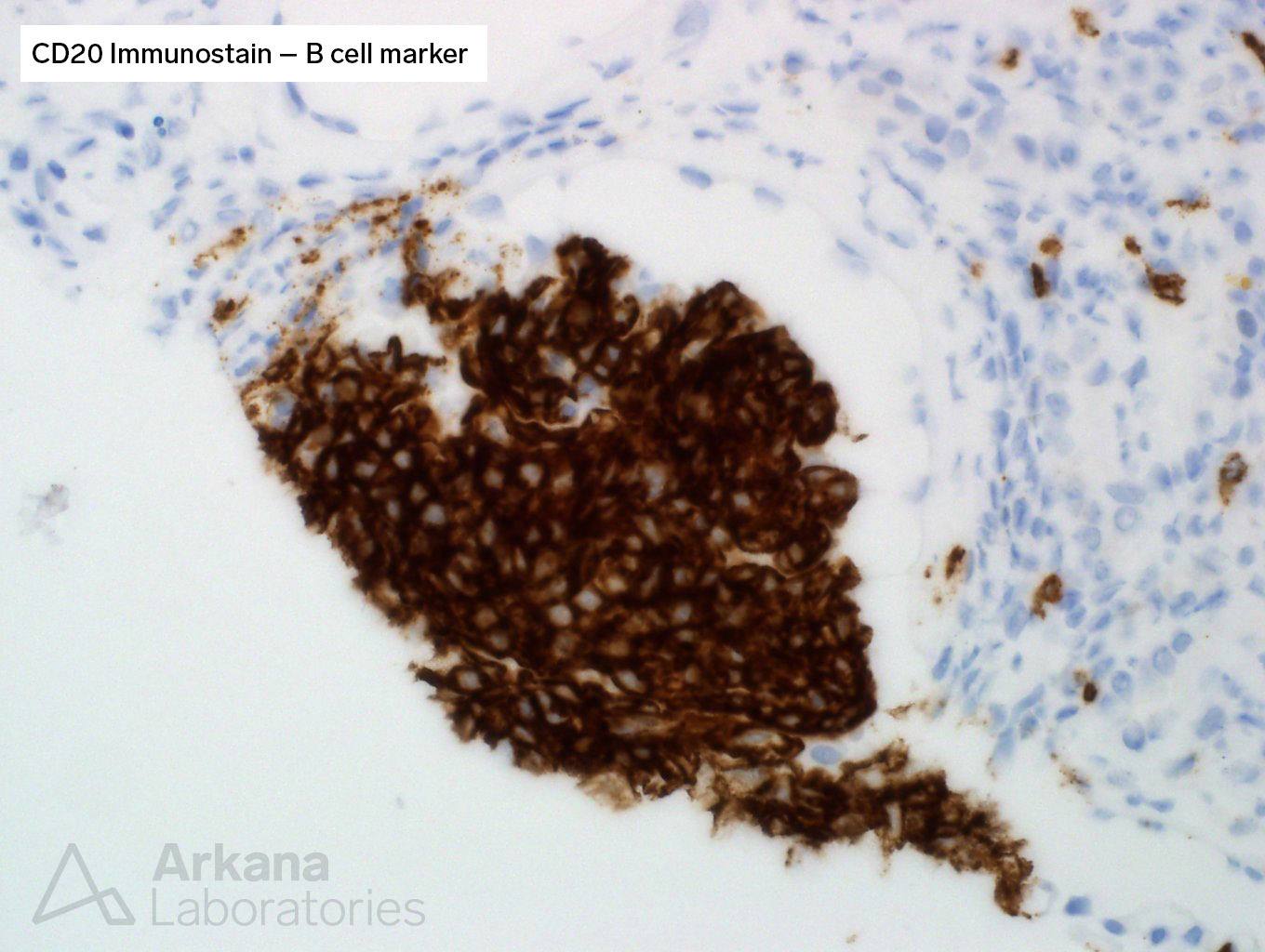
For lymphoma, CD3 (T-cell marker) and CD20 (B-cell marker) immunostains were done.
The answer finally revealed itself as the cells were strongly and uniformly positive for CD20, a marker of B-cells. And, in this context, characteristic of B-cell lymphoma.
Ockham’s razor cut us badly here, but our logical struggle was not as bad as the unfortunate diagnosis this patient received. This cancer is rare and has such unusual features, that often times it’s only discovered at autopsy. So, only one year after this patient received a diagnosis of colon cancer, a new diagnosis of intravascular large B-cell lymphoma was made on this renal biopsy. An unlucky strike indeed.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.