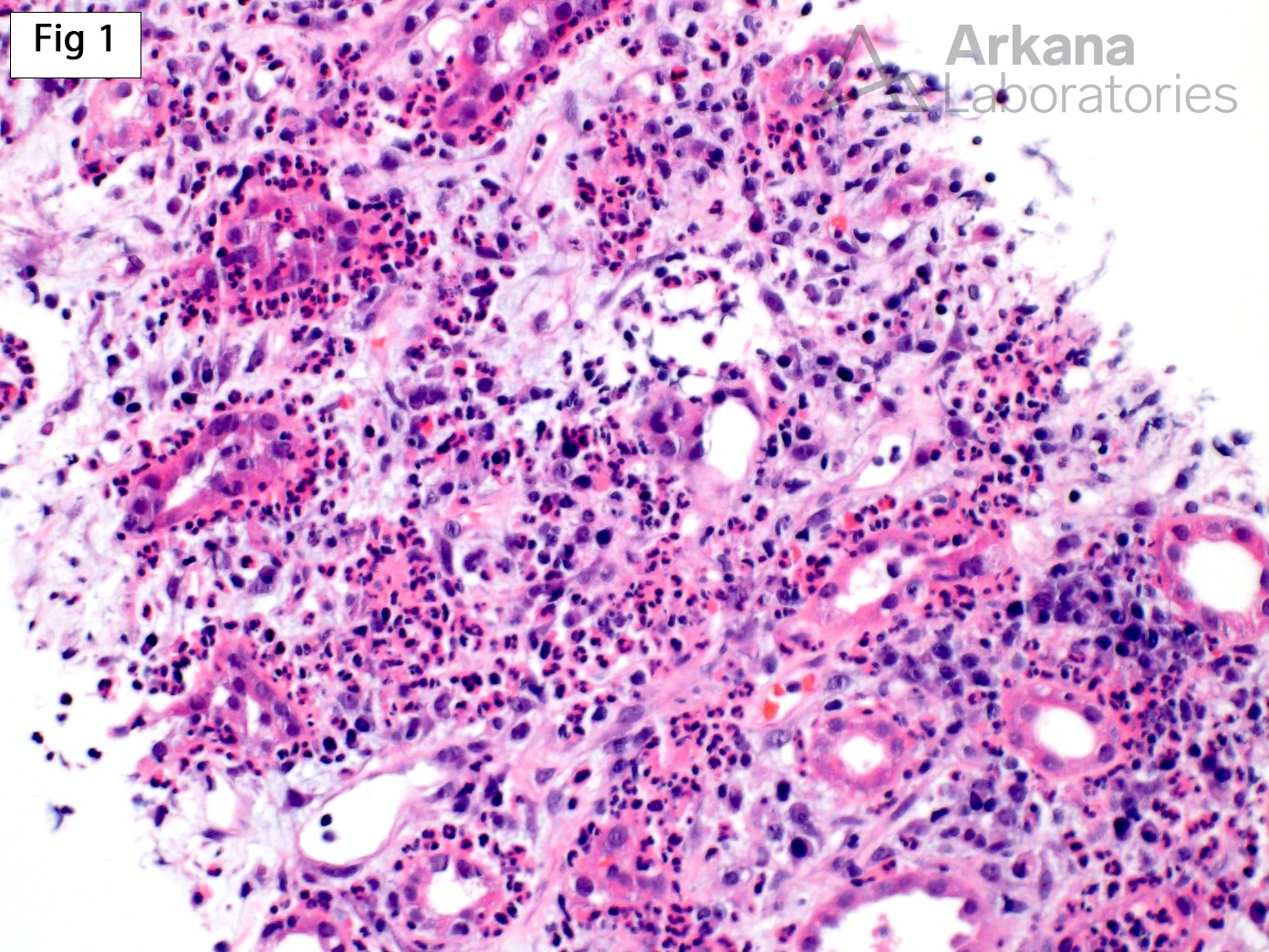
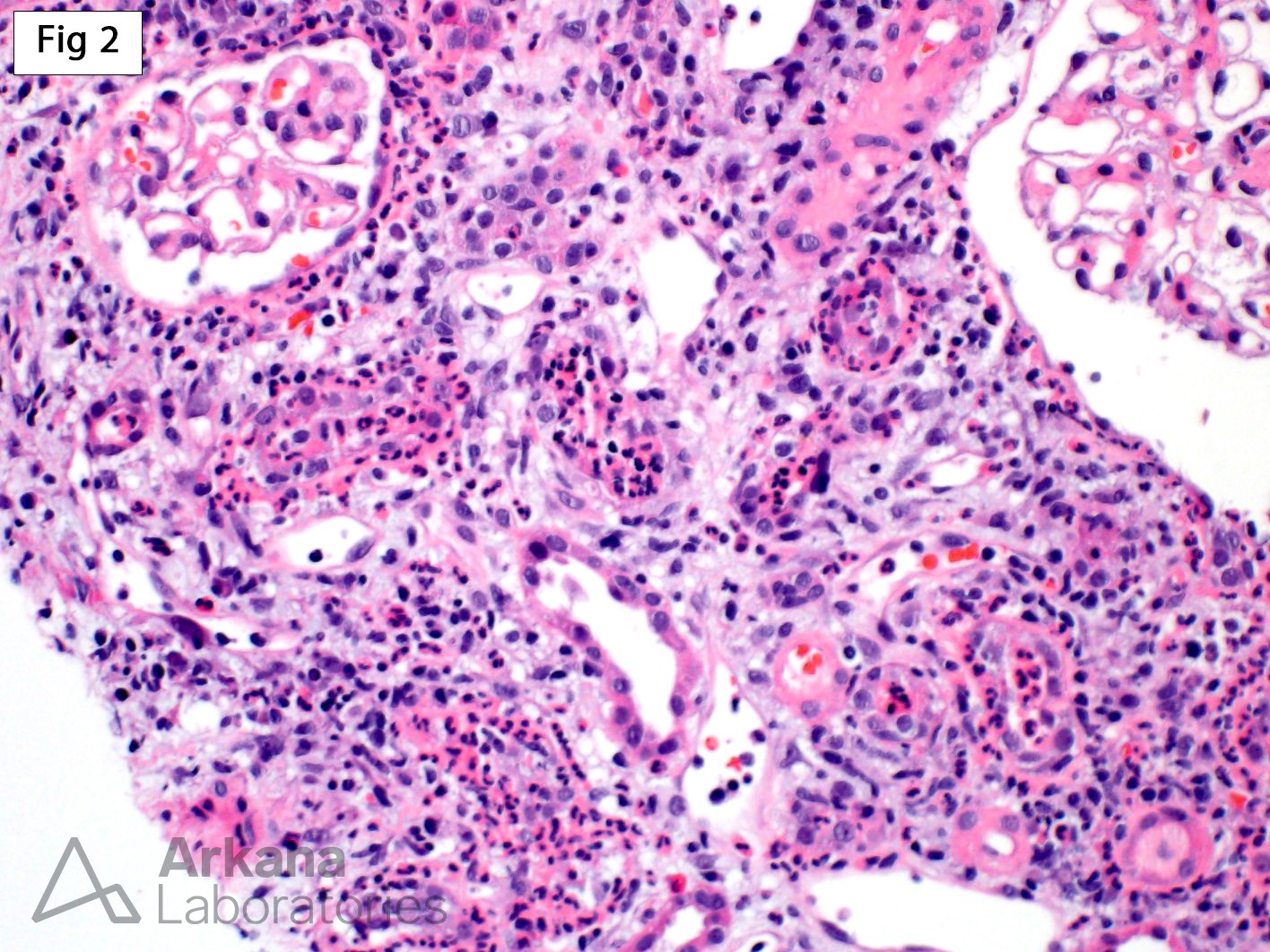
Acute pyelonephritis in transplant settings (allograft pyelonephritis) is a known cause of allograft dysfunction and a complication that occurs in approximately 10-16% of transplanted patients. Given the overlap of clinical findings between acute pyelonephritis and rejection, acute pyelonephritis is seen more often in biopsies performed on allografts than on native kidneys. This 32 year old patient presented with increased creatinine (2.6 mg/dl) 2 years after receiving a deceased donor kidney transplant. As shown in Fig 1 and 2, the biopsy shows severe neutrophilic inflammation associated with remarkable rimming of the tubules, neutrophilic tubulitis and neutrophilic casts. These features are diagnostic of acute pyelonephritis. While neutrophils may be part of the inflammatory infiltrate in acute cellular rejection, the absence of significant lymphocytes and the overwhelming predominance of neutrophils in this case, make the diagnosis of acute cellular rejection unlikely. However, occasionally features of acute pyelonephritis and acute cellular rejection may co-exist in the same allograft biopsy.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.