Clinical Presentation:
A 45-year-old male patient underwent a deceased donor renal transplantation for end-stage renal disease secondary to hypertension and type II diabetes mellitus. His postoperative course was uneventful, and he was discharged with stable kidney function. Four months post-transplant, he presented with fever, flank pain, and a decline in kidney function. A biopsy of the transplanted kidney was performed.
Renal Biopsy Findings:
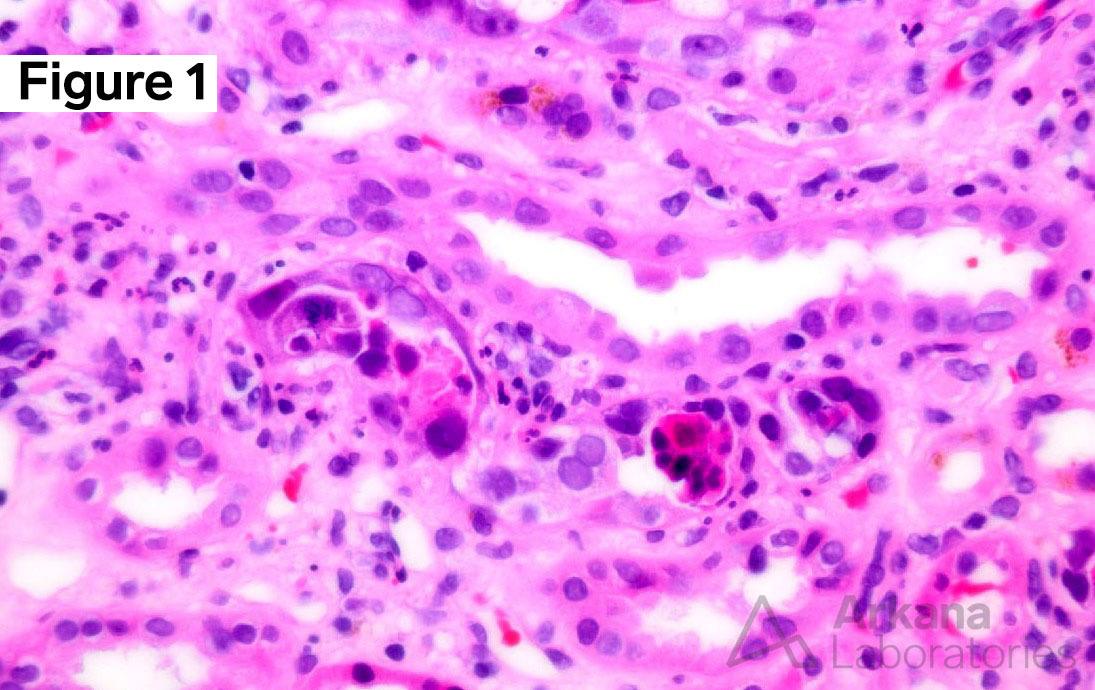
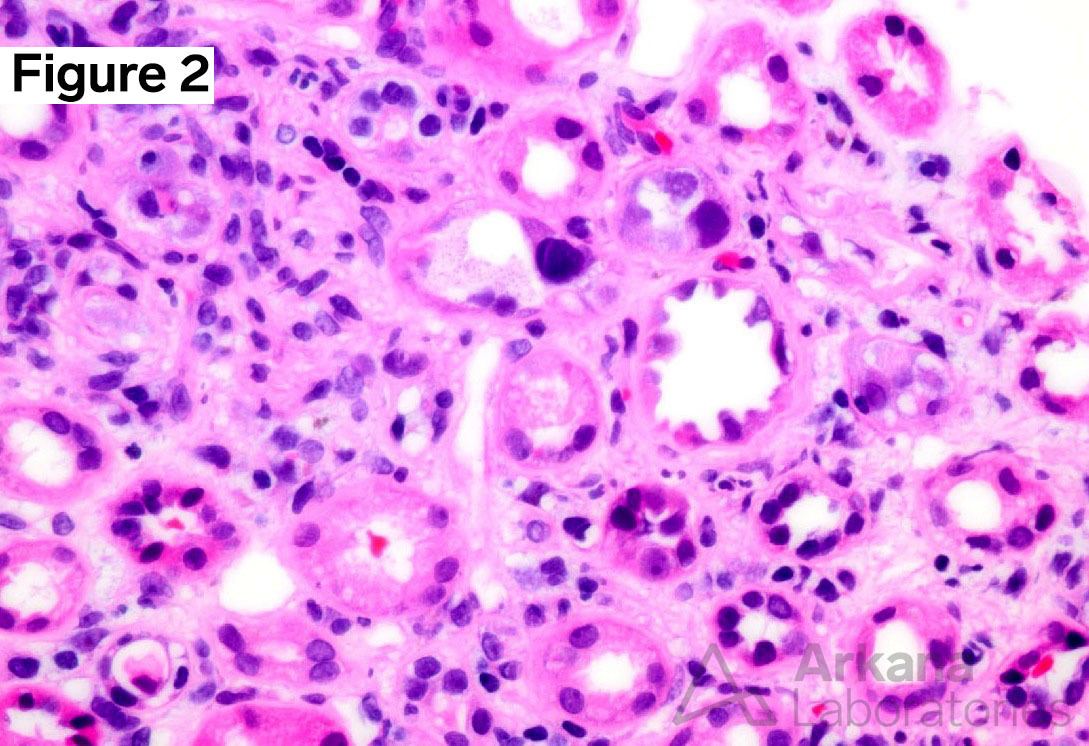
There are two main findings on renal biopsy:
- Tubular epithelial injury associated with interstitial inflammation. There is tubular epithelial cell lysis, necrosis with sloughing into the lumen, and tubulitis.
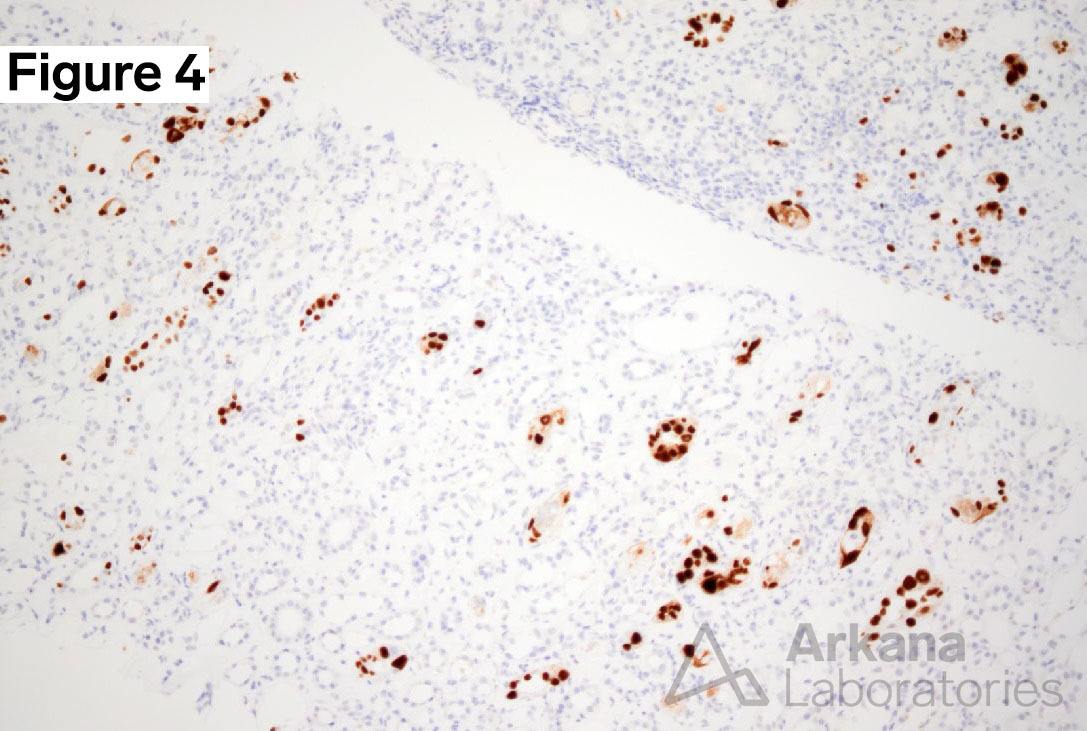
- Intranuclear viral inclusion bodies in tubular epithelial cells. Epithelial cell nuclei are reactive in appearance, and show prominent smudgy/ground glass inclusions.
Of note, the glomeruli are normal.
Additional Clues:
Diagnosis:
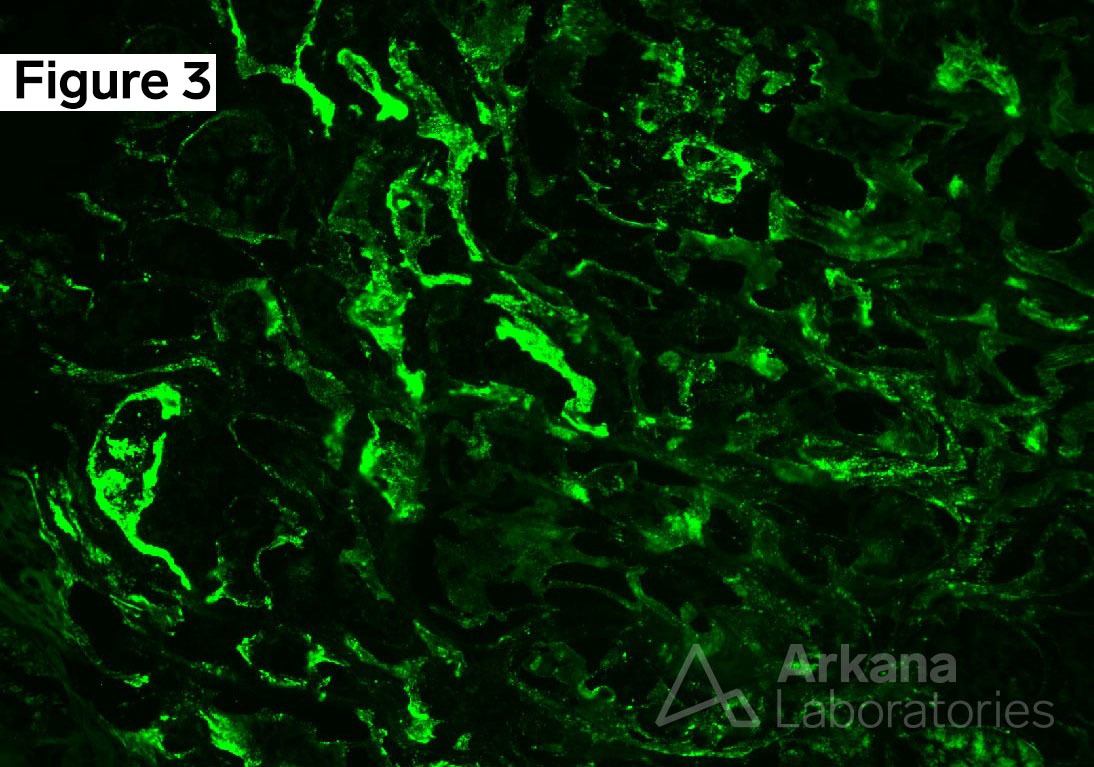
Biopsy of the transplanted kidney revealed polyomavirus nephropathy (PVN), which was confirmed by characteristic histopathological features, including tubular epithelial injury, viral inclusions, as well as positive SV40 immunohistochemistry staining. PVN is a significant complication following renal transplantation, affecting 1% to 10% of renal transplant recipients. In 5% to 50% of cases, the transplanted kidney is lost. PVN is caused by the reactivation of polyomavirus, a double-stranded DNA virus. Polyomavirus is widespread, with a prevalence of 90% in the adult population. Infection occurs during childhood and is typically asymptomatic, after which the virus establishes lifelong latency. However, the virus can reactivate in immunocompromised or immunosuppressed patients. In the setting of transplant immunosuppression, it is though that latent polyomavirus in the donor kidney is reactivated, leading to the development of PVN.
The differential diagnosis for PVN includes other viral infections, such as adenovirus and cytomegalovirus, as well as acute T-cell mediated rejection (Banff 1A or 1B), which may present with similar morphologic biopsy findings of tubular injury, interstitial inflammation and tubulitis. However, a negative SV40 stain is expected in cases of acute T-cell mediated rejection. Although rare, concurrent acute T-cell mediated rejection and PVN have been reported. The significance of tubulointerstitial basement membrane (TBM) staining for immunoglobulins and complement in some cases of PVN is currently unknown.
In conclusion, polyomavirus nephropathy is a serious complication that can occur in renal transplant recipients due to reactivation of polyomavirus. Accurate diagnosis of PVN is crucial, as it can often be mistaken for other viral infections or acute T-cell mediated rejection. It is important to note the overlapping histopathologic features on biopsy, given the vastly different treatment strategy for rejection. Early detection and prompt treatment of PVN is essential to prevent further damage to the transplanted kidney and improve patient outcomes.
References:
Colvin, Robert, B. and Anthony Chang. Diagnostic Pathology: Kidney Diseases. Available from: Elsevier eBooks+, (3rd Edition). Elsevier – OHCE, 2019.
Costa C, Cavallo R. Polyomavirus-associated nephropathy. World J Transplant. 2012;2(6):84-94.
Fogo AB, Kashgarian M. Diagnostic Atlas of Renal Pathology. 4th edition. Elsevier; 2022.
Jennette JC, Olson JL, Silva FG, D’Agati V, Heptinstall RH *1920 *, eds. Heptinstall’s Pathology of the Kidney: Includes Interactive EBook with Complete Content. Seventh edition. Wolters Kluwer; 2015.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.