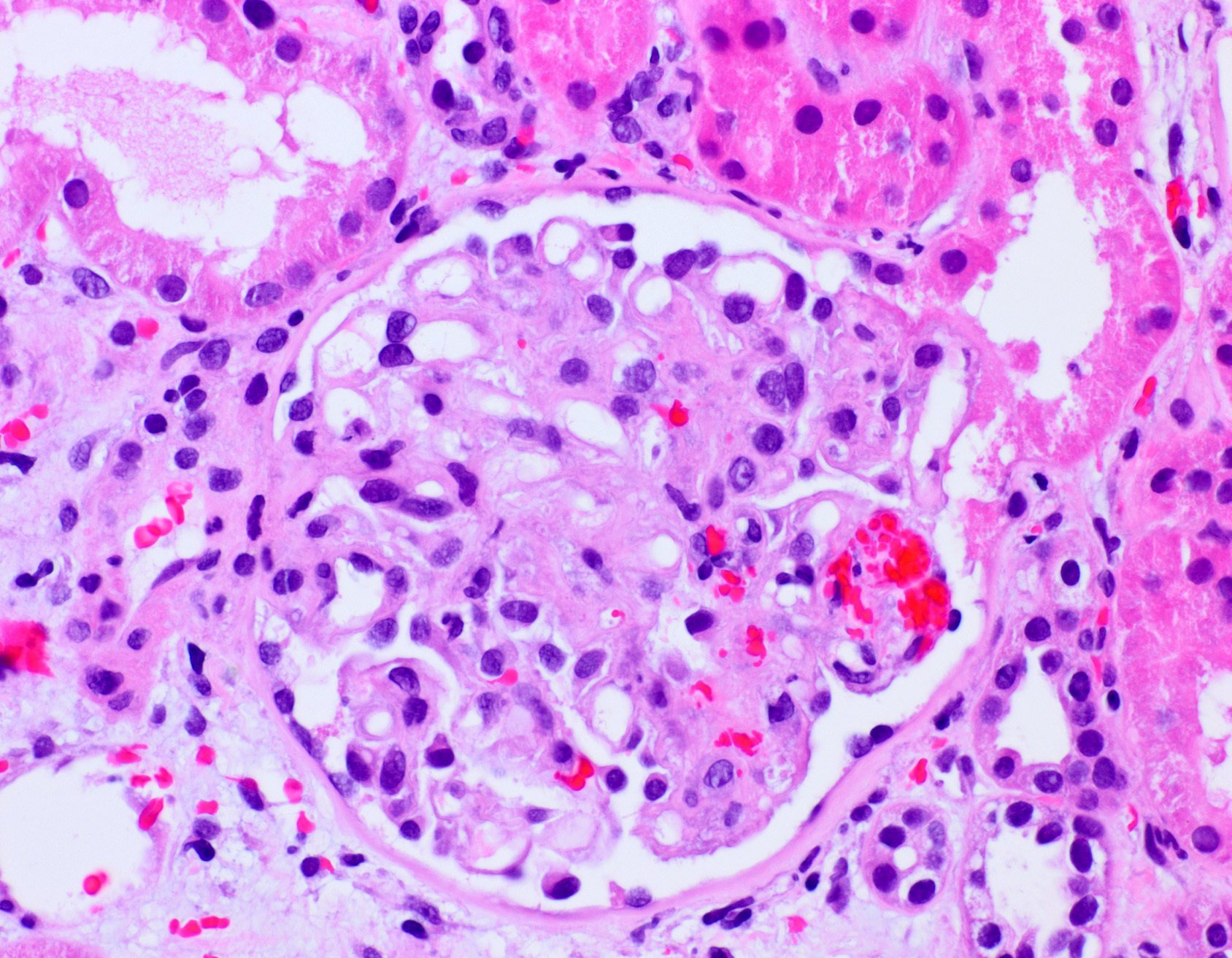
This is a 3 month post-transplant kidney biopsy from a patient with ESRD due to polycystic kidney disease. She recently developed CMV disease and AKI (Creatinine is 5.4 from a baseline of 1.4mg.dl). What is your diagnosis?
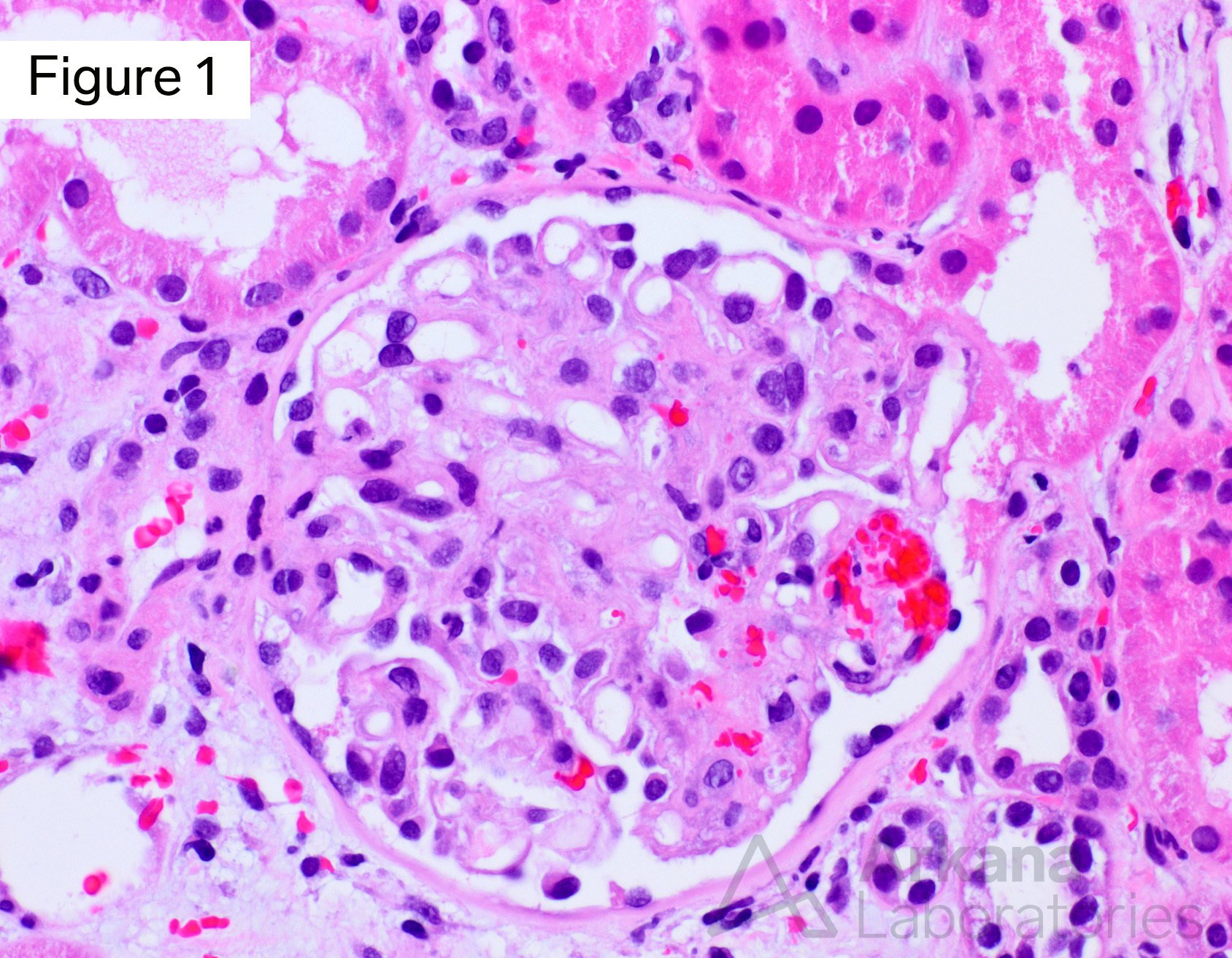
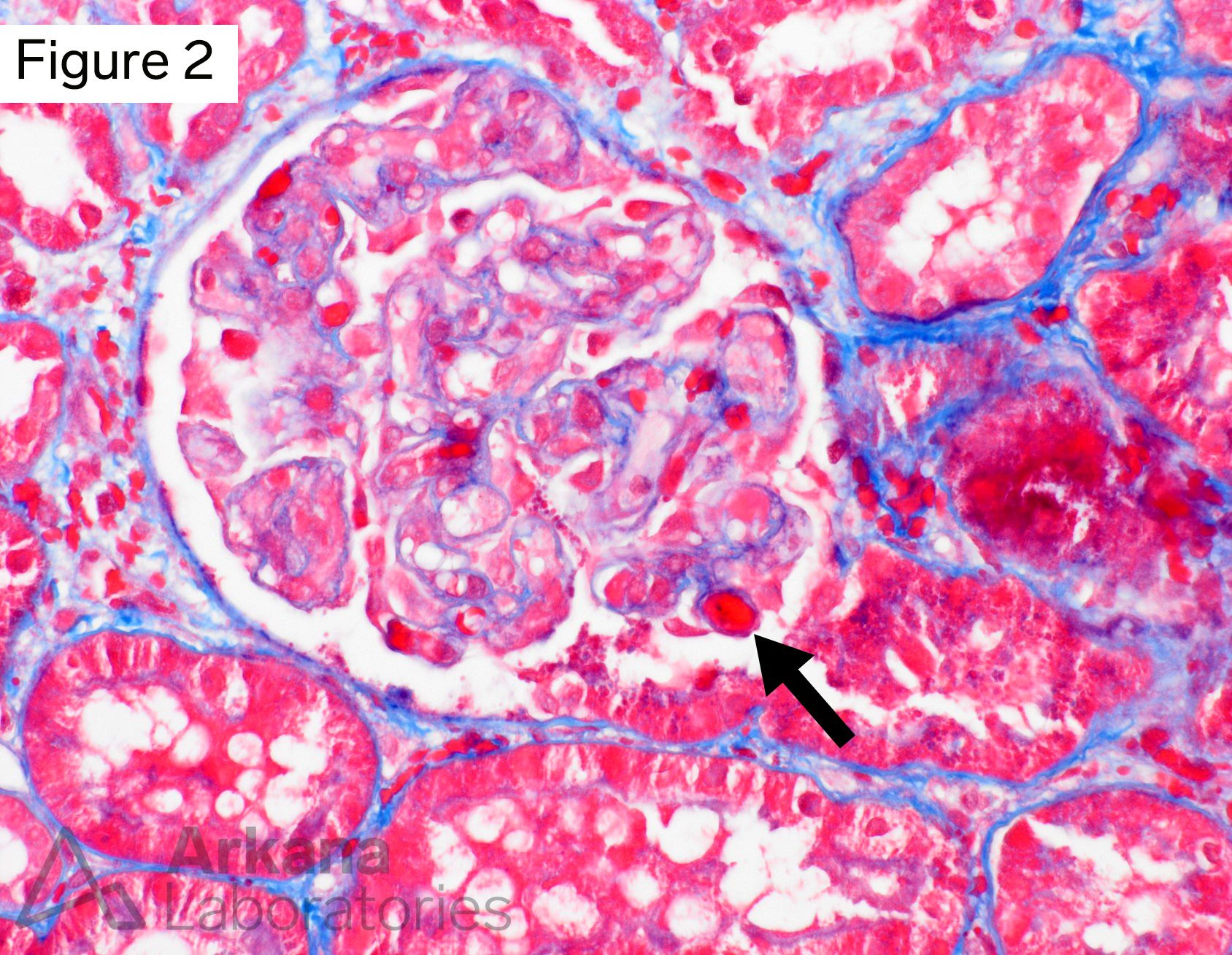
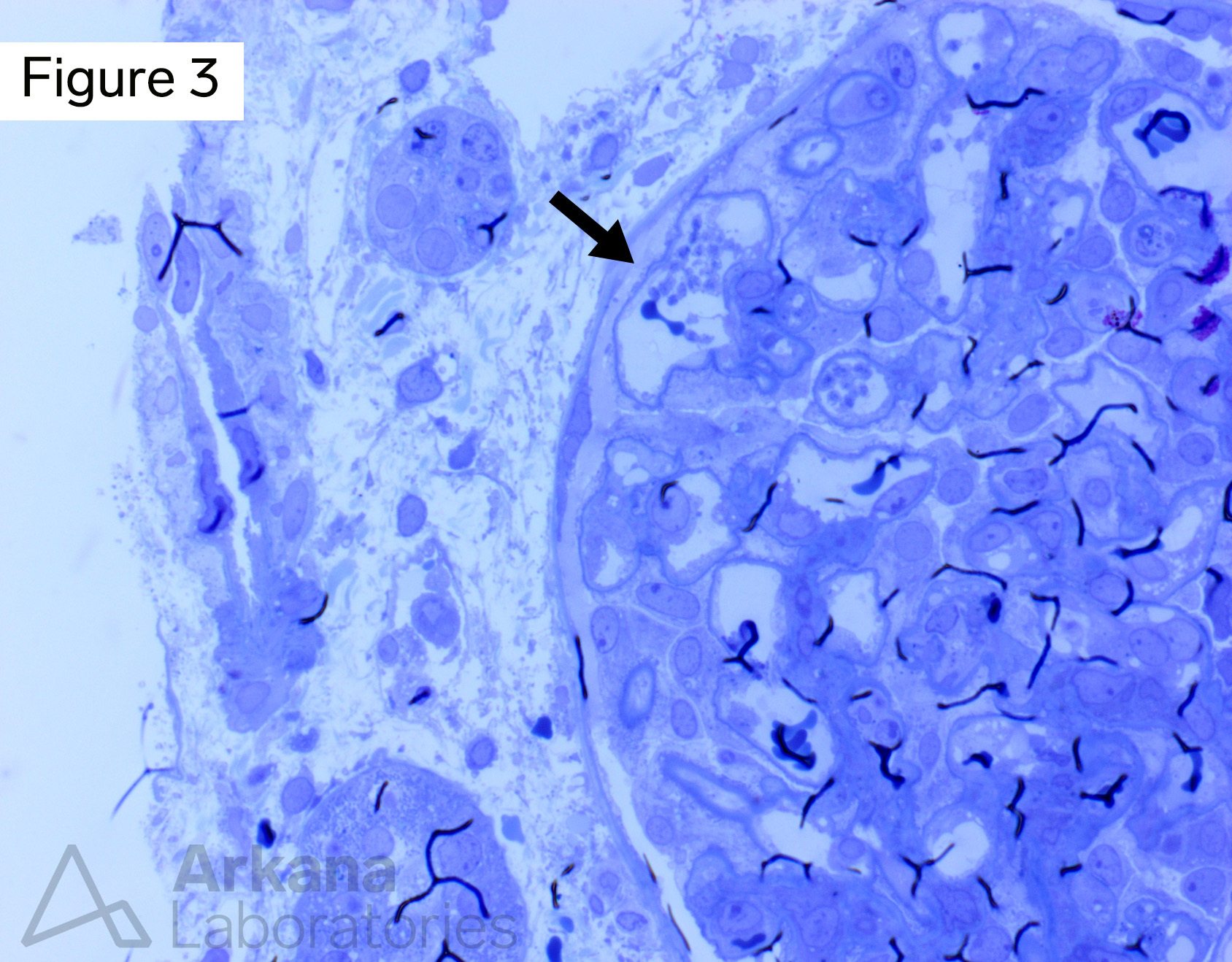
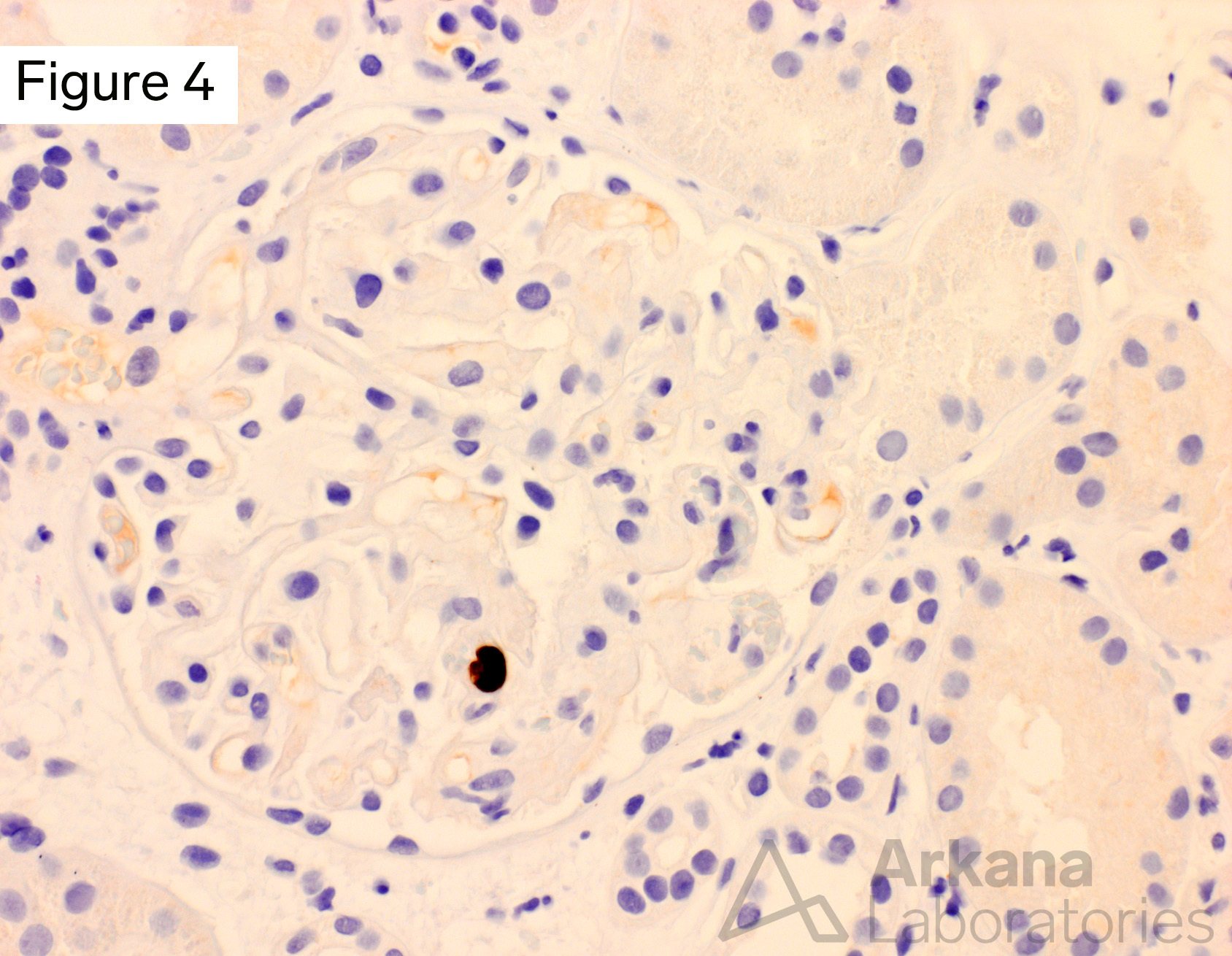
The image shows a glomerulus with mesangiolysis and fragmented red blood cells, consistent with microangiopathic changes. Elsewhere, small thrombi (Figure 2, trichrome) and platelet aggregates were seen (Figure 3, toluidine blue). Due to the history of CMV disease, a CMV immunohistochemical stain was performed and was positive within a single glomerular endothelial cell (Figure 4).
Thrombotic microangiopathy can have numerous etiologies, all of which show morphologic overlap. These include accelerated hypertension, scleroderma renal crisis, antiphospholipid antibody syndrome, drugs (including calcineurin inhibitors), disorders of complement regulation (atypical HUS), infections, ADAMTS 13 abnormalities, and malignancy, among others. In the transplant setting, the differential diagnosis also includes antibody-mediated rejection. This patient did not have donor specific antibodies, there was no microvascular inflammation, and C4d stain was negative. It is possible that the recent CMV infection was a trigger for the development of TMA in this case, as this has been previously described in a few transplant recipients (https://pubmed.ncbi.nlm.nih.gov/25864519/).
Java A, Edwards A, et al. Cytomegalovirus-induced thrombotic microangiopathy after renal transplant successfully treated with eculizumab: case report and review of the literature. Transpl Int. 2015 Sep;28(9):1121-5.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.