Clinical History
The patient is a 52-year-old man presents with decreased vision, left eye, double vision, lagging of left eyelid, severe headaches/retro-orbital pain. Prior left temporal, skull base mass. Status-post resection and gamma knife 9 years ago. Imaging showed recurrent mass with adjacent bony destruction
Question:
Bony destruction most likely excludes the following diagnosis?
A. Meningioma
B. Hemangiopericytoma
C. Langerhans cell histiocytosis
D. Metastatic carcinoma
Answer:
Bony destruction most likely excludes the following diagnosis?
A. Meningioma
Meningiomas usually show adjacent hyperostosis
– Thought to signify bony invasion by meningioma
– Meningioma may be primarily intraosseous
– Not associated with grade, brain invasion, or recurrence
All other choices usually present with bony destruction.
Final Diagnosis: Anaplastic hemangiopericytoma, WHO grade 3
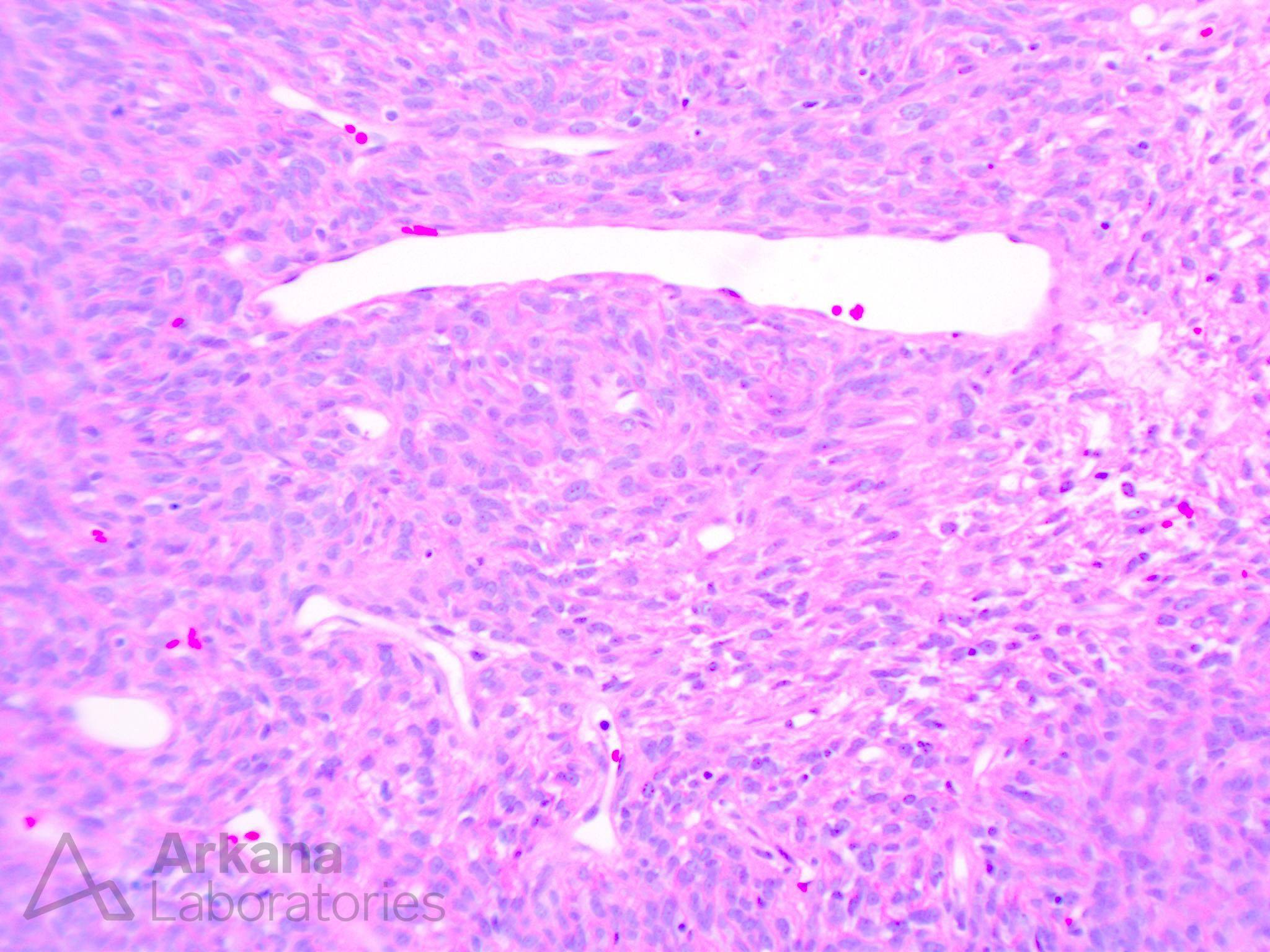
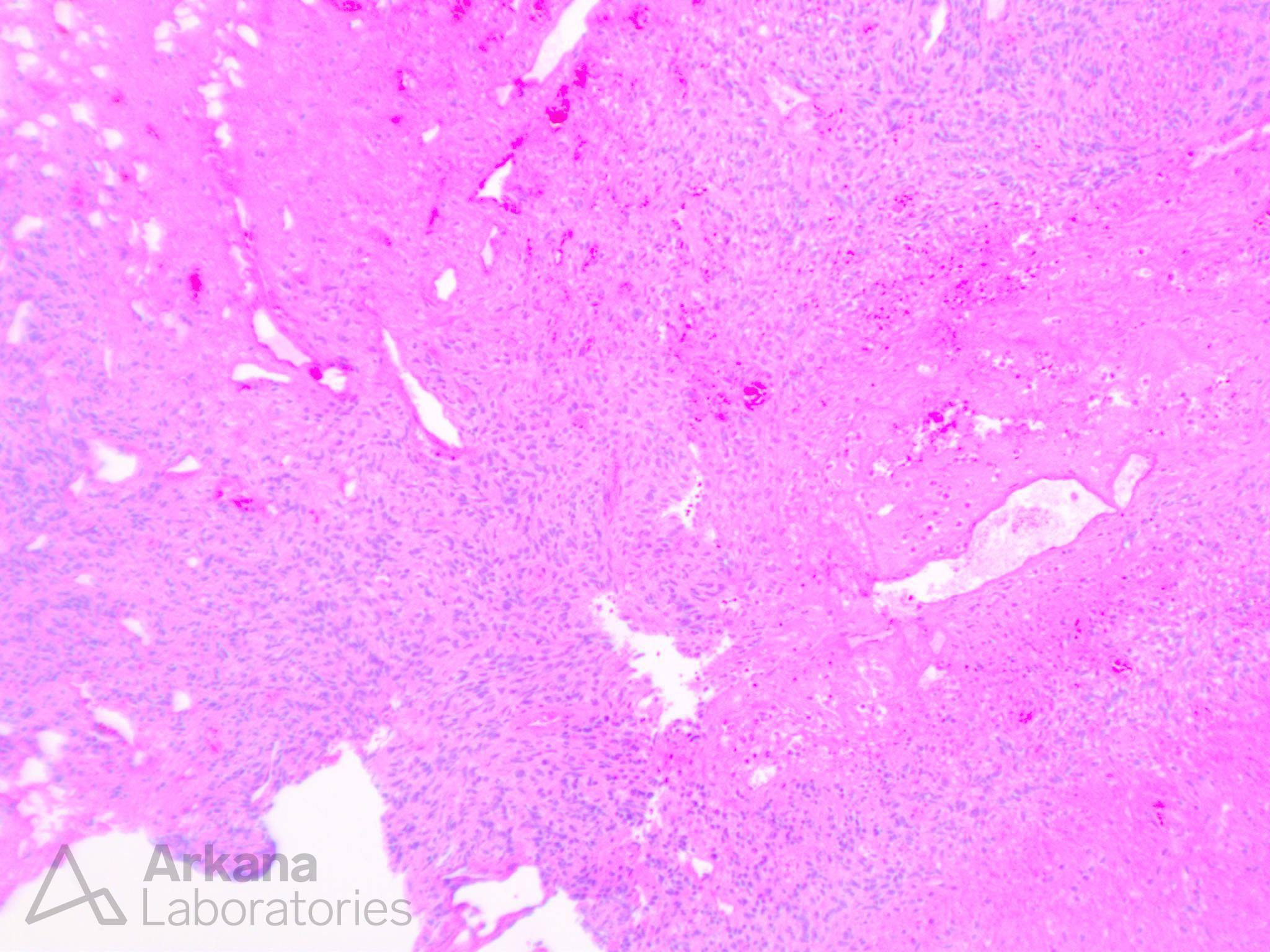
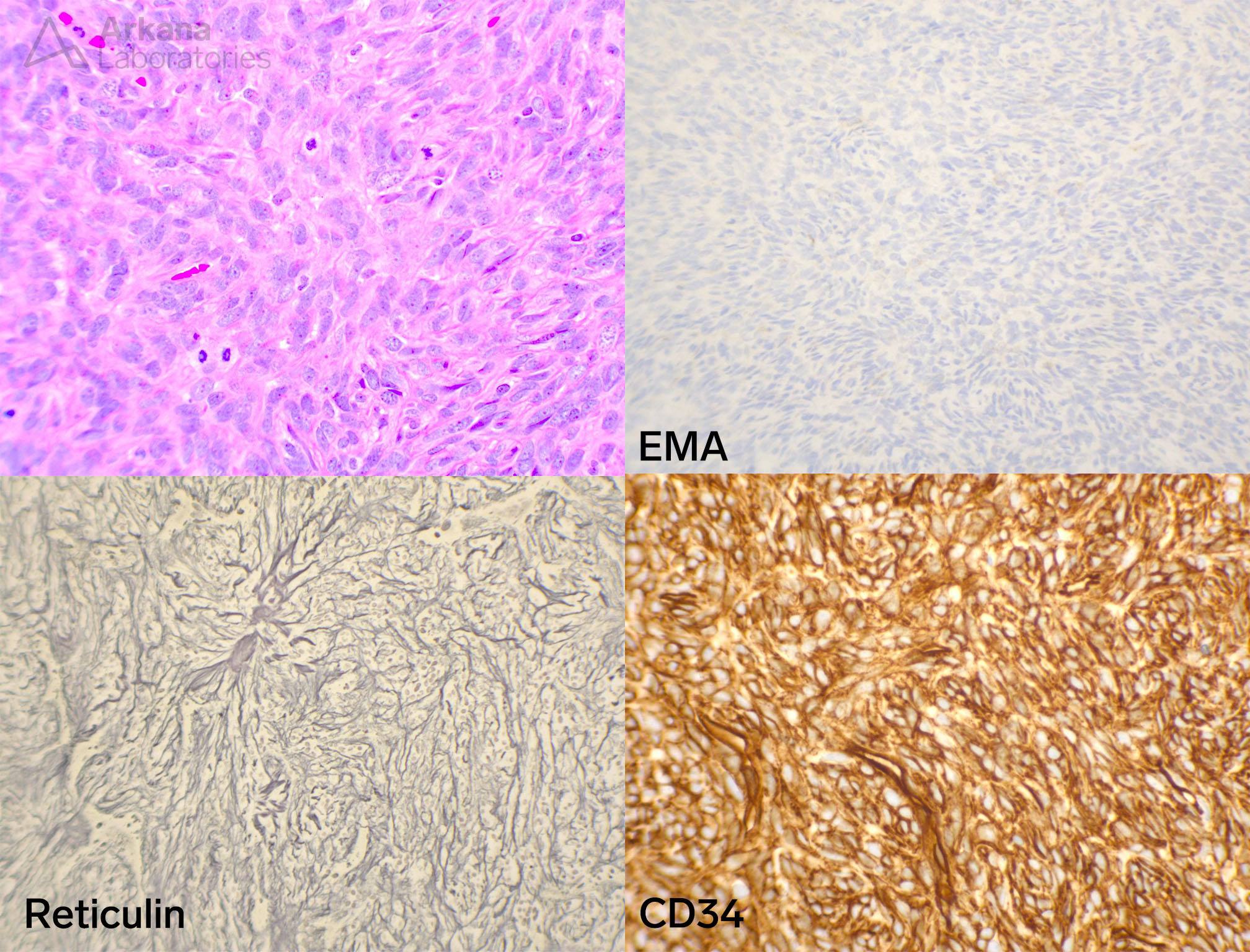
SFT histology
Variably hypercellular, plump spindled neoplastic cells with elongated nuclei and occasional nucleoli
Sheets and occasional poorly formed fascicles
Thin-walled, “staghorn” vessels
Special stains: reticulin-rich, CD34+, EMA-
STAT6 nuclear positivity is currently required for diagnosis
Anaplastic features
Elevated mitotic activity (>5/10 hpf here)
Necrosis
Hypercellularity
Hemorrhage
Reference(s) / additional reading:
Takase H, Yamamoto T. Bone Invasive Meningioma. Front Oncol. 2022;12:895374.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.