Clinical History
This 65-year-old patient presented with bilateral symmetrical proximal upper and lower extremity muscle weakness, dysphagia and skin rash. Their past medical history was significant for recent diagnosis of renal cell carcinoma (status post resection). Laboratory studies showed elevated CPK (625) and aldolase (20). Myositis specific autoantibody panel test results are pending.
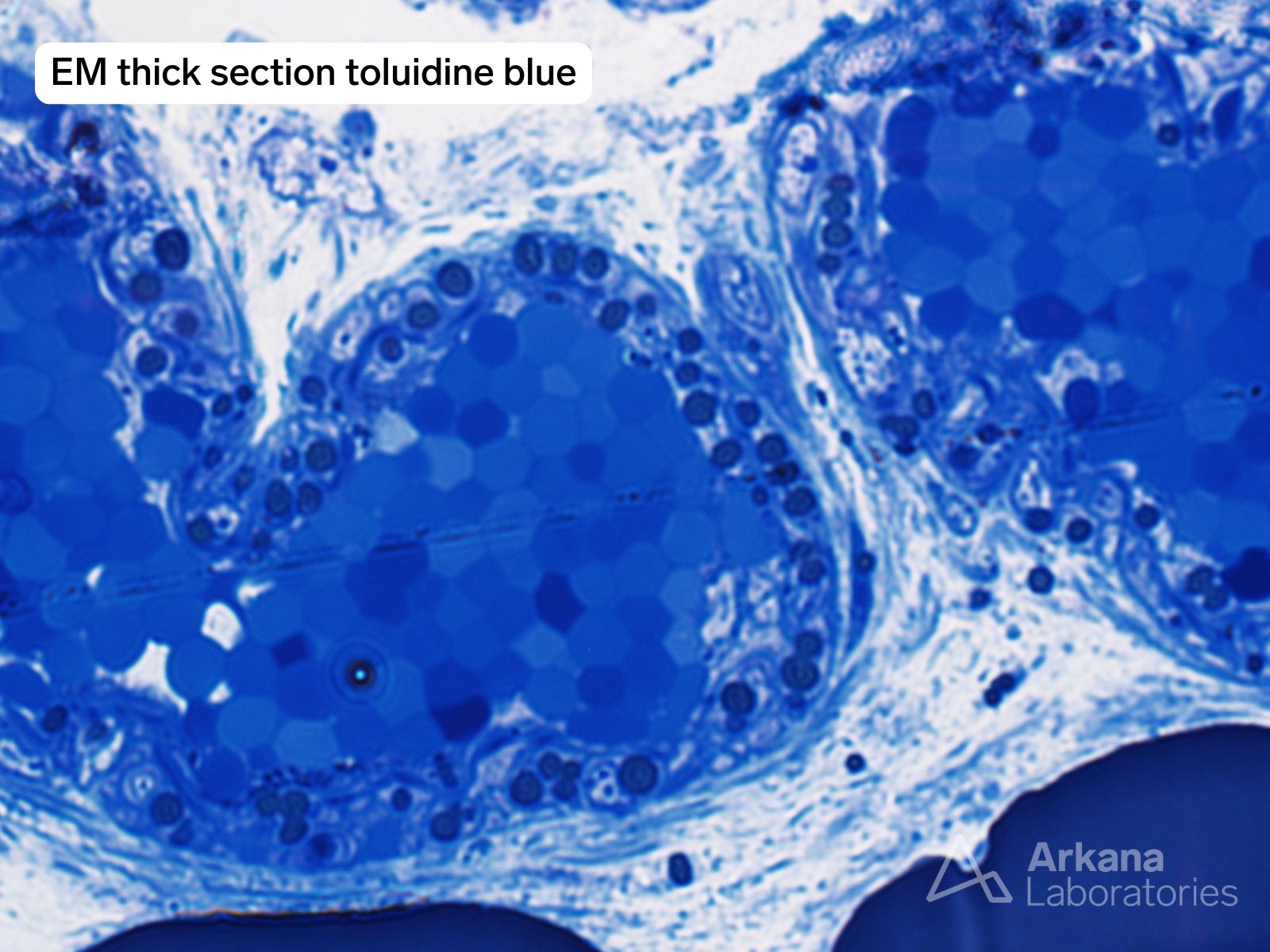
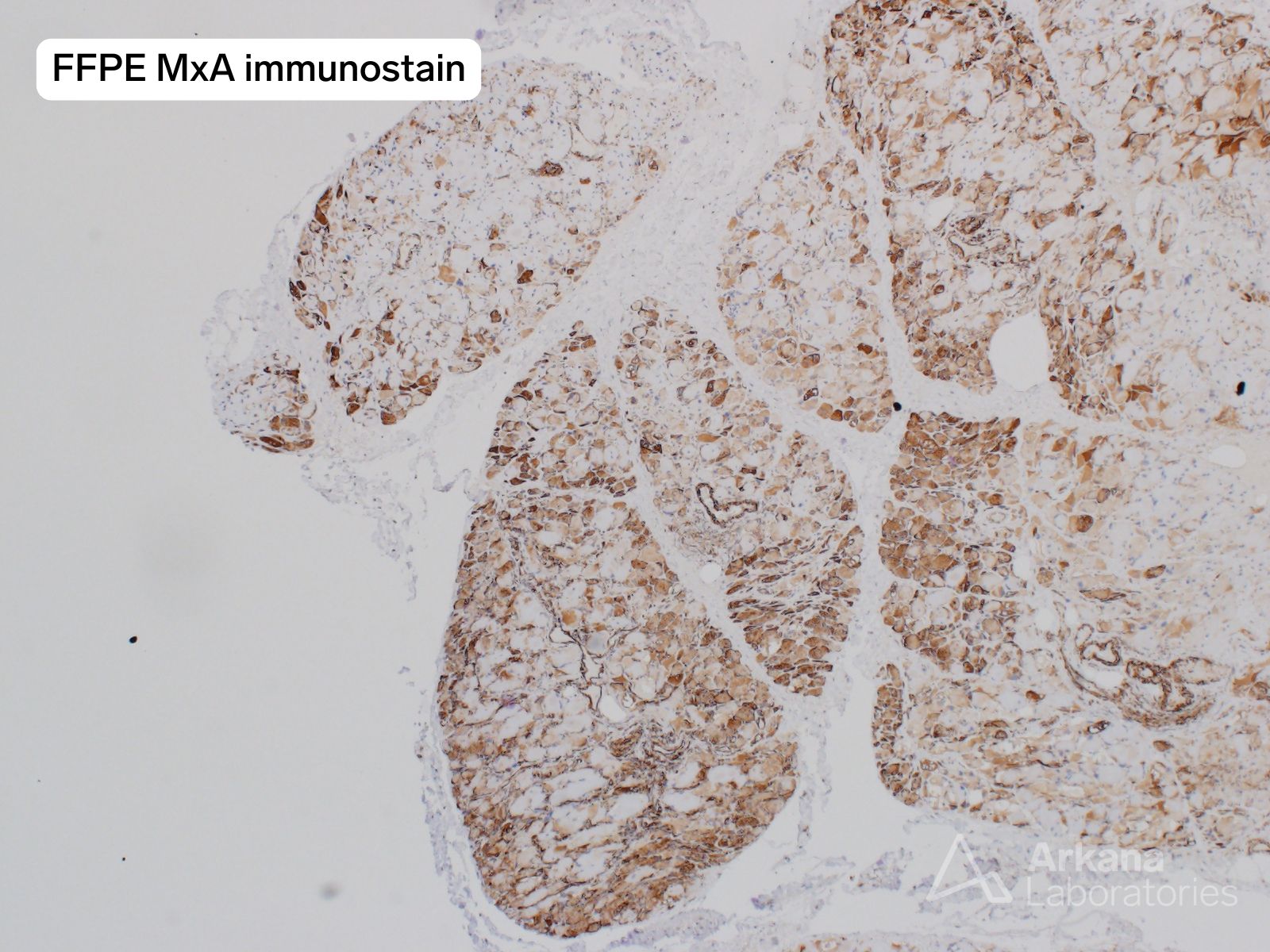
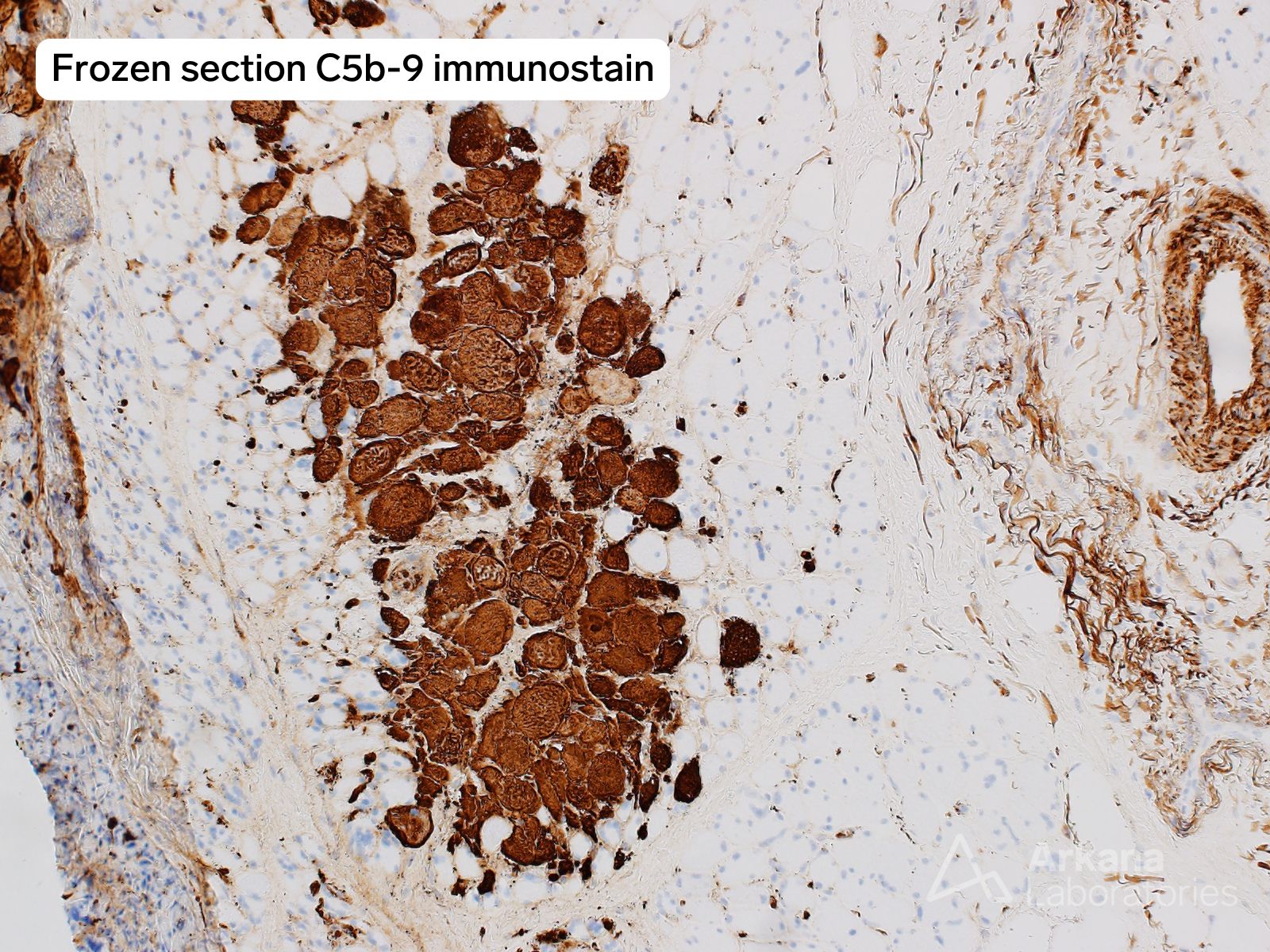
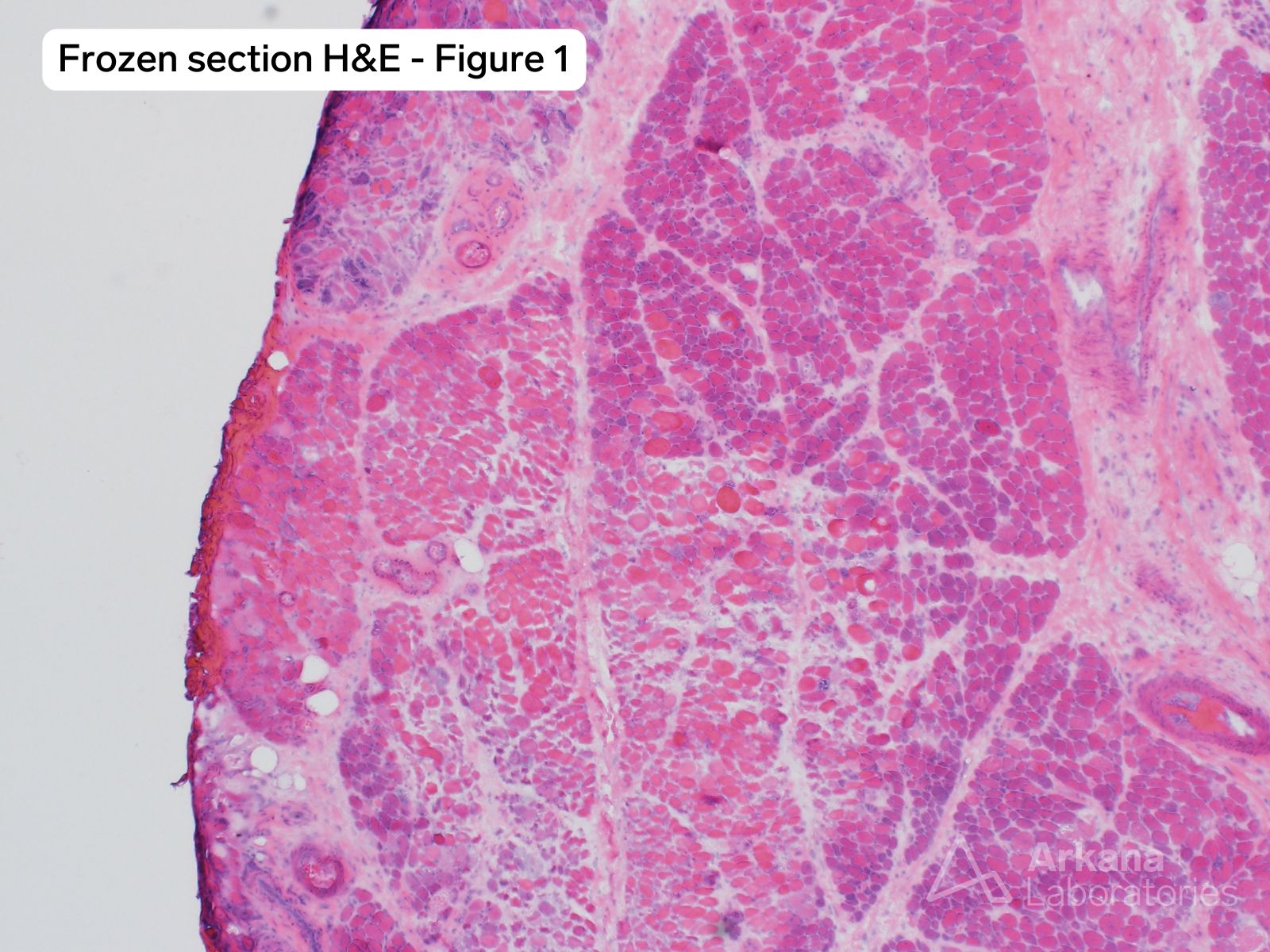
What is your diagnosis based on the provided H&E, MxA and C5b-9 images? What abnormality does the Oil-red-O stain (ORO) and Toluidine blue stained thick section images demonstrate?
Correct Answer:
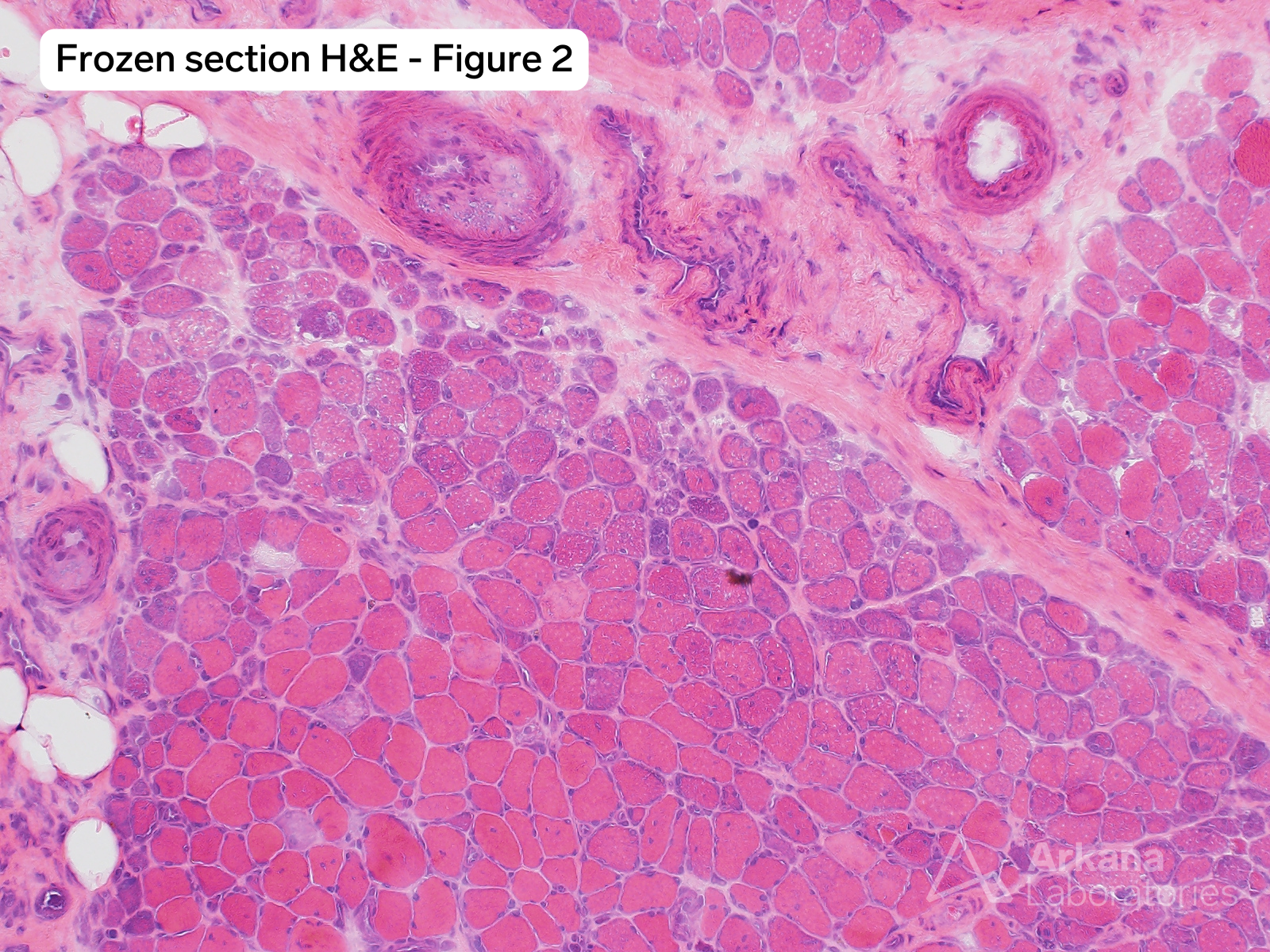
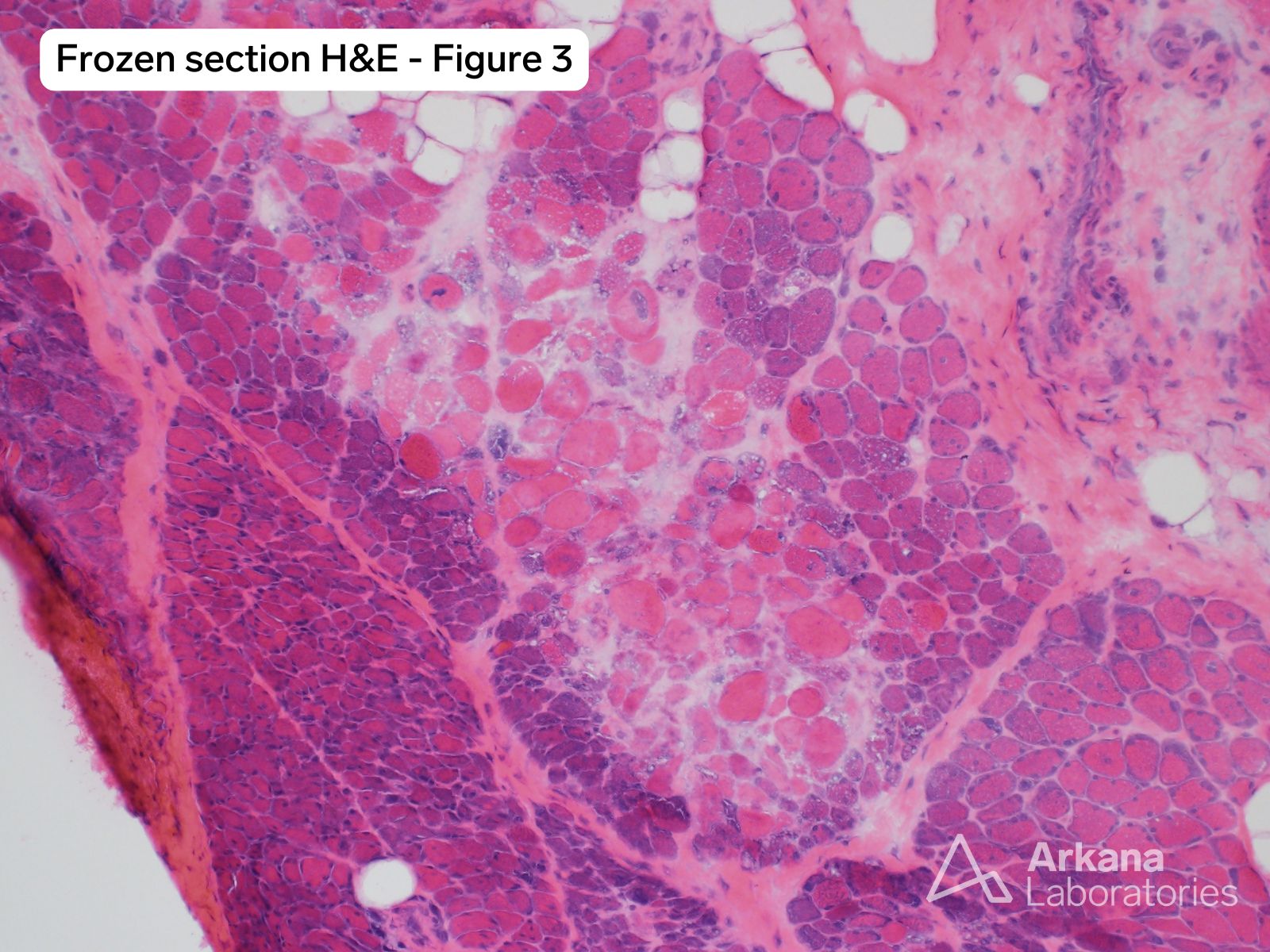
The muscle biopsy shows pathologic alterations of an active myopathic process with areas of geographic myofiber necrosis involving adjacent fascicles as well as areas of geographic myofiber necrosis involving the central region of fascicles. Patchy perifascicular pattern of myofiber injury also appears to be present. The perimysial fibrous connective tissue is increased and shows increased cellularity due to the presence of macrophages. Occasional perimysial blood vessels show evidence of vascular injury. MxA immunostain shows diffuse and perifascicular patterns of myofiber staining. C5b-9 immunostain highlights the areas of myonecrosis. In the context of this patient’s clinical history these alterations are consistent with the presence of a paraneoplastic dermatomyopathy which has been designated “Regional Ischemic Immune Myopathy / RIIM).” Regional infarction may also be seen in dermatomyositis related to NXP2 and TIF1-gamma autoantibodies, which also has a stronger association with malignancy.
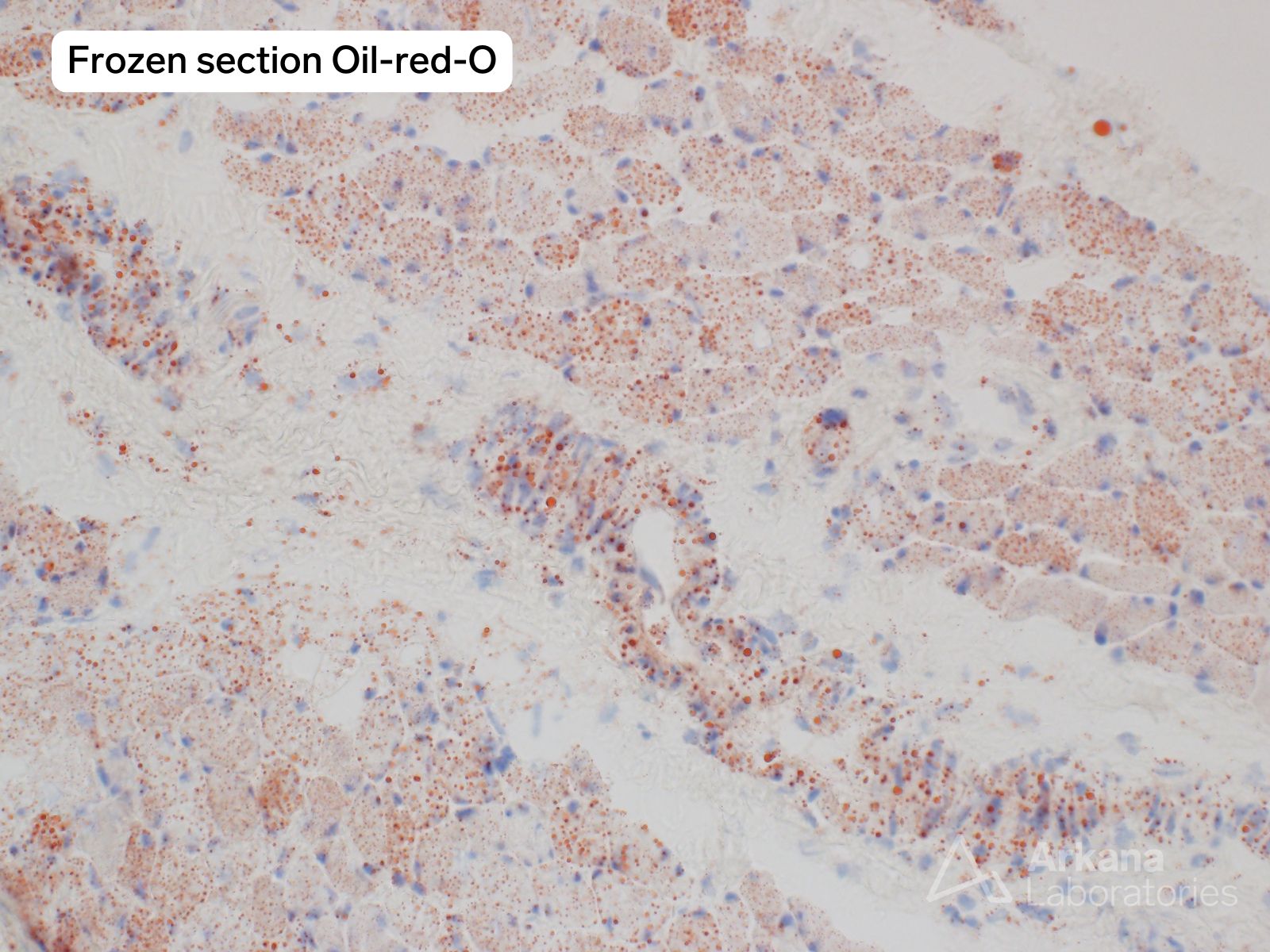
The ORO stain showed significant increase in myofiber lipid and the presence of lipid within small blood vessel walls. This latter feature is also demonstrated on the thick section. Variable lipid accumulation within myofibers may be seen in inflammatory and immune-mediated myopathies, and is suspected to represent a secondary alteration possibly due to mitochondrial dysfunction. Variable accumulation of lipid within the blood vessel walls may also be seen. It is of potential interest that dyslipidemia in the setting of juvenile dermatomyositis has recently been reported to correlate with disease activity.
References:
-
-
Cai C, Alshehri A, Choksi R, Pestronk A. Regional ischemic immune myopathy: a paraneoplastic dermatomyopathy. J Neuropathol Exp Neurol. 2014 Dec;73(12):1126-33. doi: 10.1097/NEN.0000000000000132. PMID: 25383636.
-
Tanboon J, Inoue M, Saito Y, Tachimori H, Hayashi S, Noguchi S, Okiyama N, Fujimoto M, Nishino I. Dermatomyositis: Muscle Pathology According to Antibody Subtypes. Neurology. 2022 Feb 15;98(7):e739-e749. doi: 10.1212/WNL.0000000000013176. Epub 2021 Dec 6. PMID: 34873015; PMCID: PMC8865893.
-
Khojah A, Morgan G, Kadakia A, Klein-Gitelman MS, Pachman LM. Dyslipidemia in Juvenile Dermatomyositis. Sci Rep. 2024 Nov 3;14(1):26528. doi: 10.1038/s41598-024-77985-4. PMID: 39489760; PMCID: PMC11532421.
-
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.