Clinical History
This 40-year-old patient presented with progressive proximal upper and lower extremity muscle weakness (difficulty ascending stairs and lifting arms) and dysphagia. Laboratory studies showed elevated CPK (>20000), CRP and ESR, and positive Jo-1 and SSA. CT of the chest demonstrated interstitial lung disease. MRI demonstrated edema of the muscles. On physical examination skin thickening and hyperkeratosis of their palms was present (“Mechanic’s hands”). The patient was treated with steroid and hydroxychloroquine prior to muscle biopsy, and reported some improvement in symptoms and partial resolution of CPK elevation.
Question
Based on figures #1-#3, which of the following is the most likely diagnosis?
A. Anti-synthetase syndrome
B. Sarcoidosis
C. Denervation
D. Polymyosistis
Answer
The answer is A. Anti-synthetase syndrome.
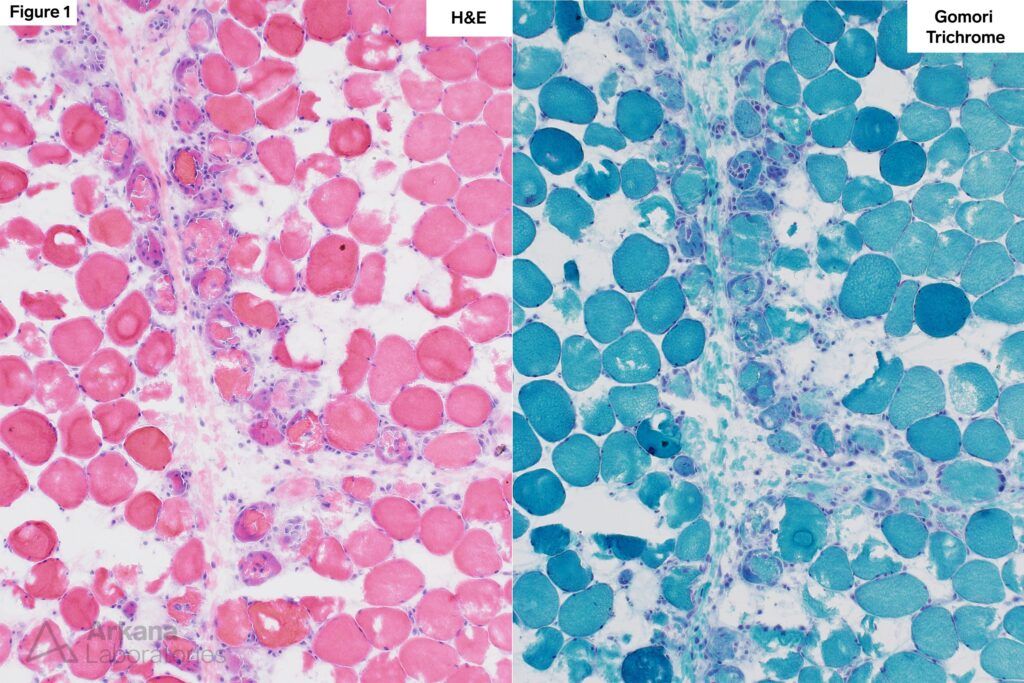
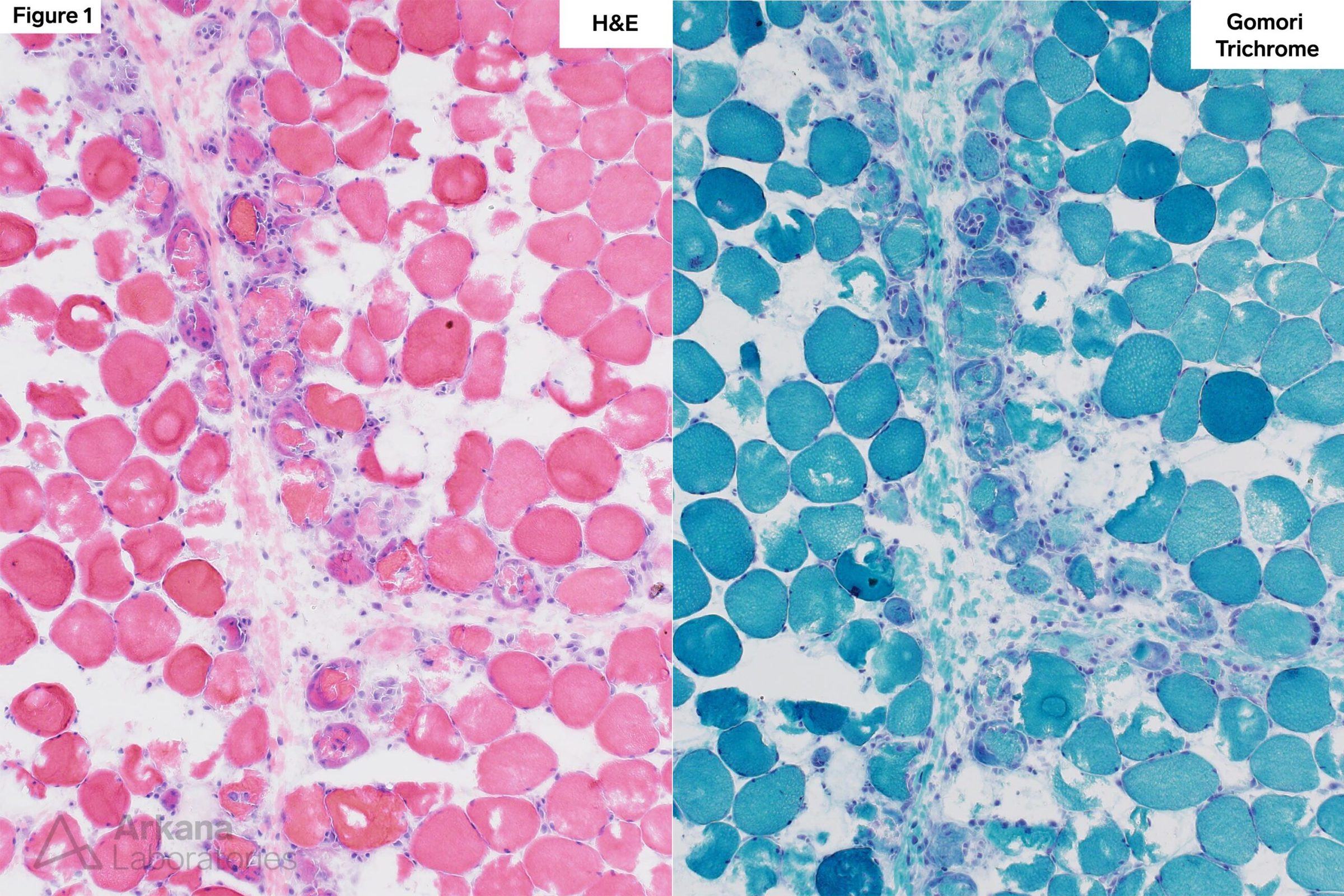
Figure 1: Frozen Section
Medium magnification image of H&E and modified Gomori Trichrome stained sections show frequent basophilic regenerating, partially necrotic and necrotic myofibers in a perifascicular distribution.
The amount of associated chronic lymphoid inflammation is limited (discordant with the degree of muscle fiber injury) and likely reflects that the patient was treated with steroid prior to muscle biopsy.
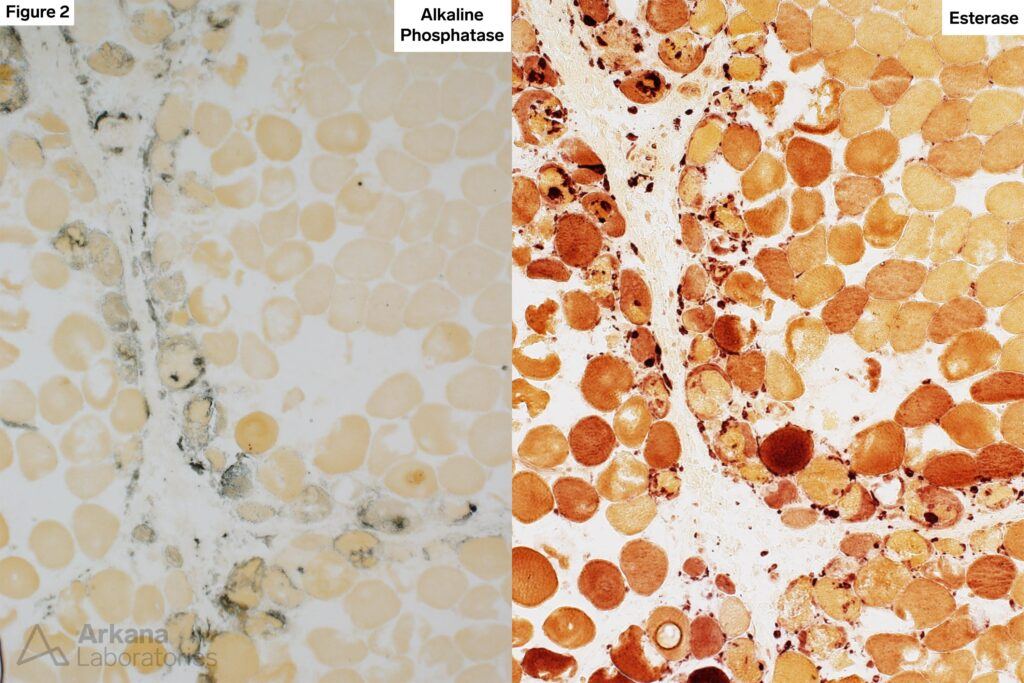
Figure 2: Frozen Section
Medium magnification image of alkaline phosphatase enzyme histochemical stain shows variable staining of the regenerating and necrotic myofibers.
Esterase enzyme histochemical stain highlights macrophages seen in association with necrotic muscle fibers, perimysial and superficial endomysial connective tissue.
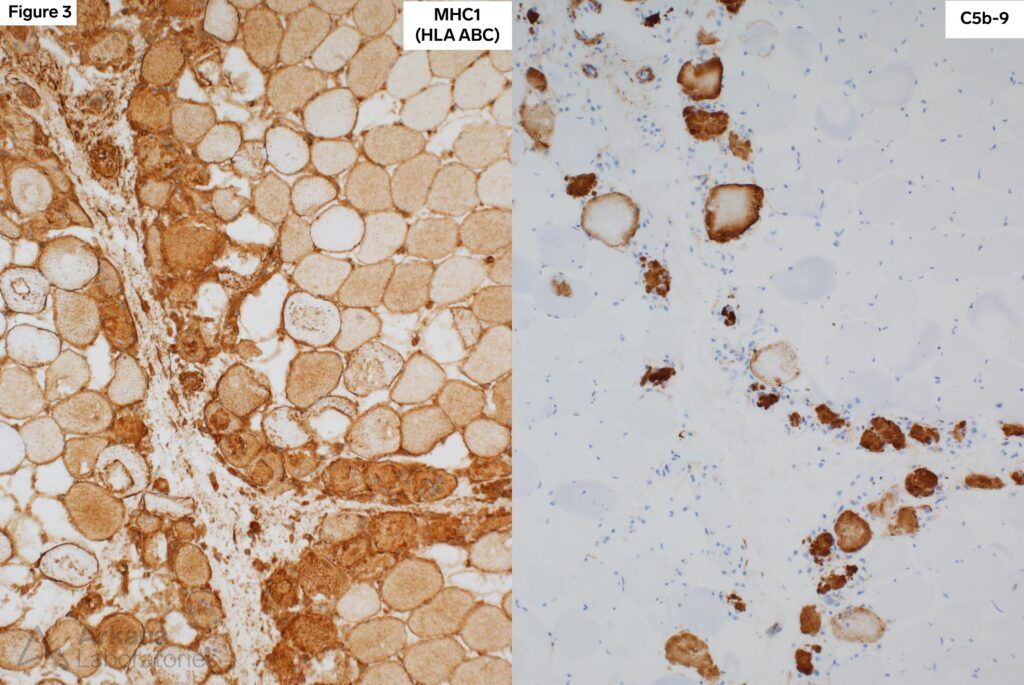
Figure 3: Frozen Section
Medium magnification image of MHC1 (Major Histocompatibility Complex I / HLA ABC) immunohistochemical stain shows diffuse increase in muscle fiber staining with accentuation of staining with accentuation of staining in a perifascicular distribution.
Medium magnification image of C5b-9 (complement membrane attack complex) immunohistochemical stain shows sarcoplasmic staining of necrotic muscle fibers in a perifascicular distribution.
Anti-synthetase Syndrome
- Anti-synthetase syndrome is associated with an increased risk of interstitial lung disease. Patient often have skin changes involving their hands (Mechanic’s hands).
- Autoantibodies to aminoacyl-tRNA synthetases (ARS) are a characteristic finding in anti-synthetase syndrome. These include Jo-1 (histidyl), PL7 (threonyl), PL12 (alanyl), EJ (glycyl), OJ (isoleucyl), KS (asparaginyl), Zo (Phenylalanyl), Ha (tyrosyl), SC (lysyl), JS (glutaminyl) and YRS (tyrosyl). Jo-1 is the most common autoantibody.
- Muscle biopsies from patients with anti-synthetase syndrome frequently show patchy to well-developed perifascicular atrophy/perifascicular necrosis. In contrast to dermatomyositis which also classically shows perifascicular pattern of muscle fiber injury, anti-synthetase syndrome typically does not show positive immunostaining for MxA (myxovirus resistance protein A).
Reference(s) / Additional Reading:
Witt LJ, Curran JJ, Strek ME. The Diagnosis and Treatment of Antisynthetase Syndrome. Clin PulmMed. 2016 Sep;23(5):218-226. doi: 10.1097/CPM.0000000000000171. PMID: 27594777; PMCID: PMC5006392.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.

