The patient is a 65-year-old African American female who presents with a protein/creatinine ratio of 2 and a serum creatinine of 3.5 mg/dl. Serologies for ANA, dsDNA, c-ANCA, p-ANCA, and rheumatoid factor are negative. On CT examination, she has several enlarged peribronchial lymph nodes. Her ACE level is elevated.
What is the best diagnosis?
A. Necrotizing Vasculitis.
B. Acute Interstitial Nephritis Concerning for a Drug Reaction.
C. Granulomatous Interstitial Nephritis Concerning for Sarcoidosis.
D. ANCA-associated Vasculitis with Diffuse Crescents.
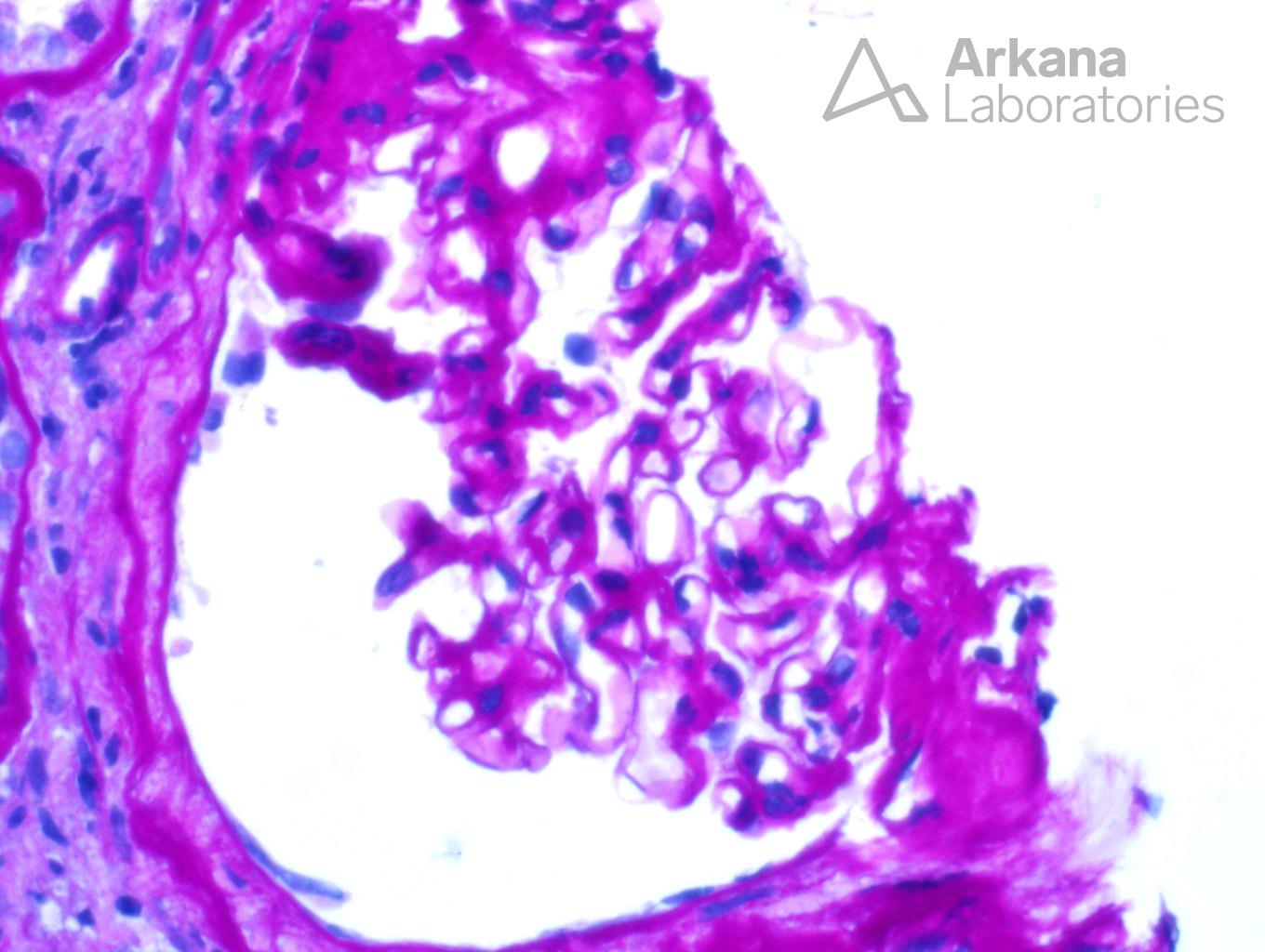
The correct answer is c: Granulomatous Interstitial Nephritis Concerning for Sarcoidosis.
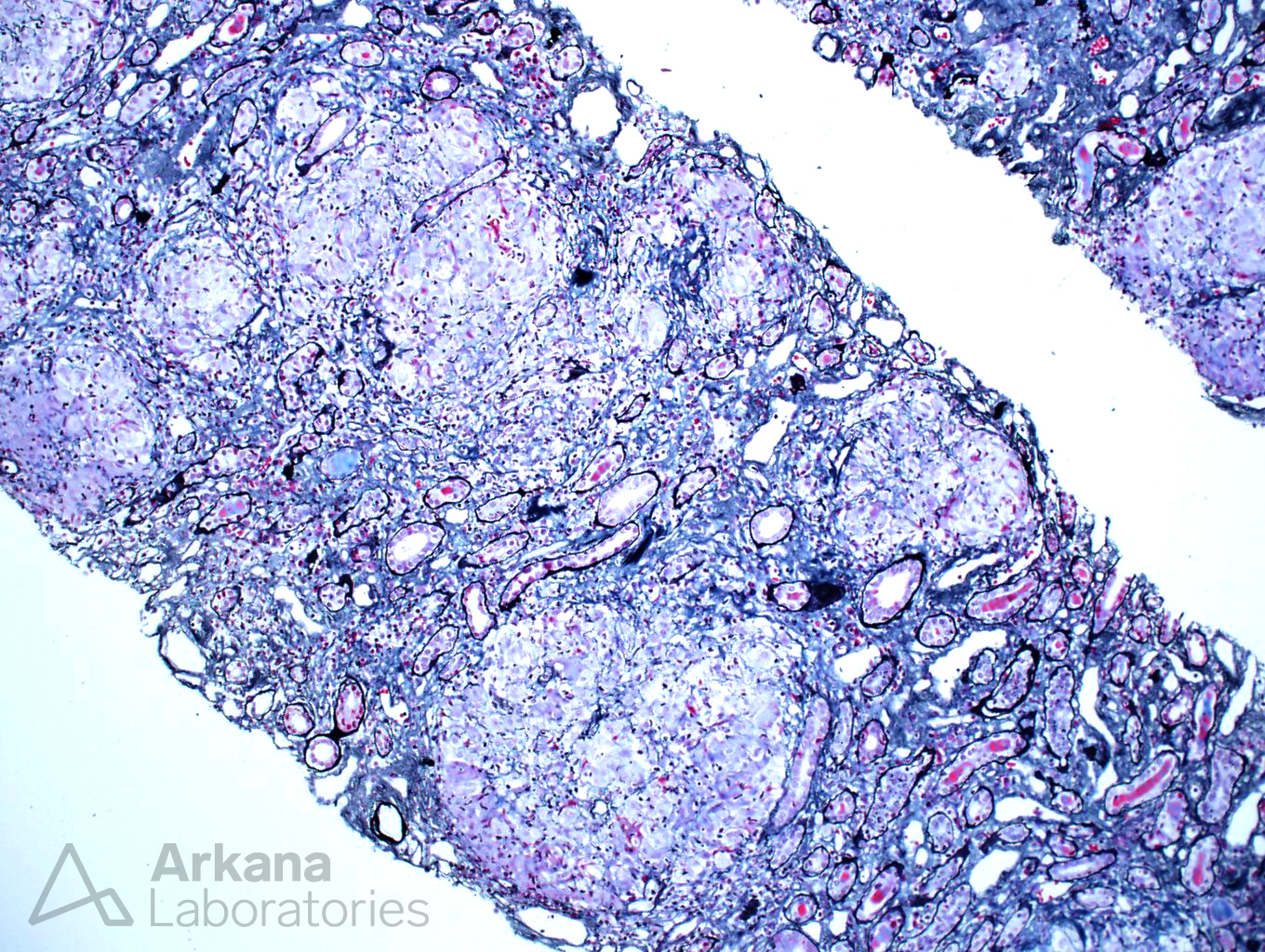
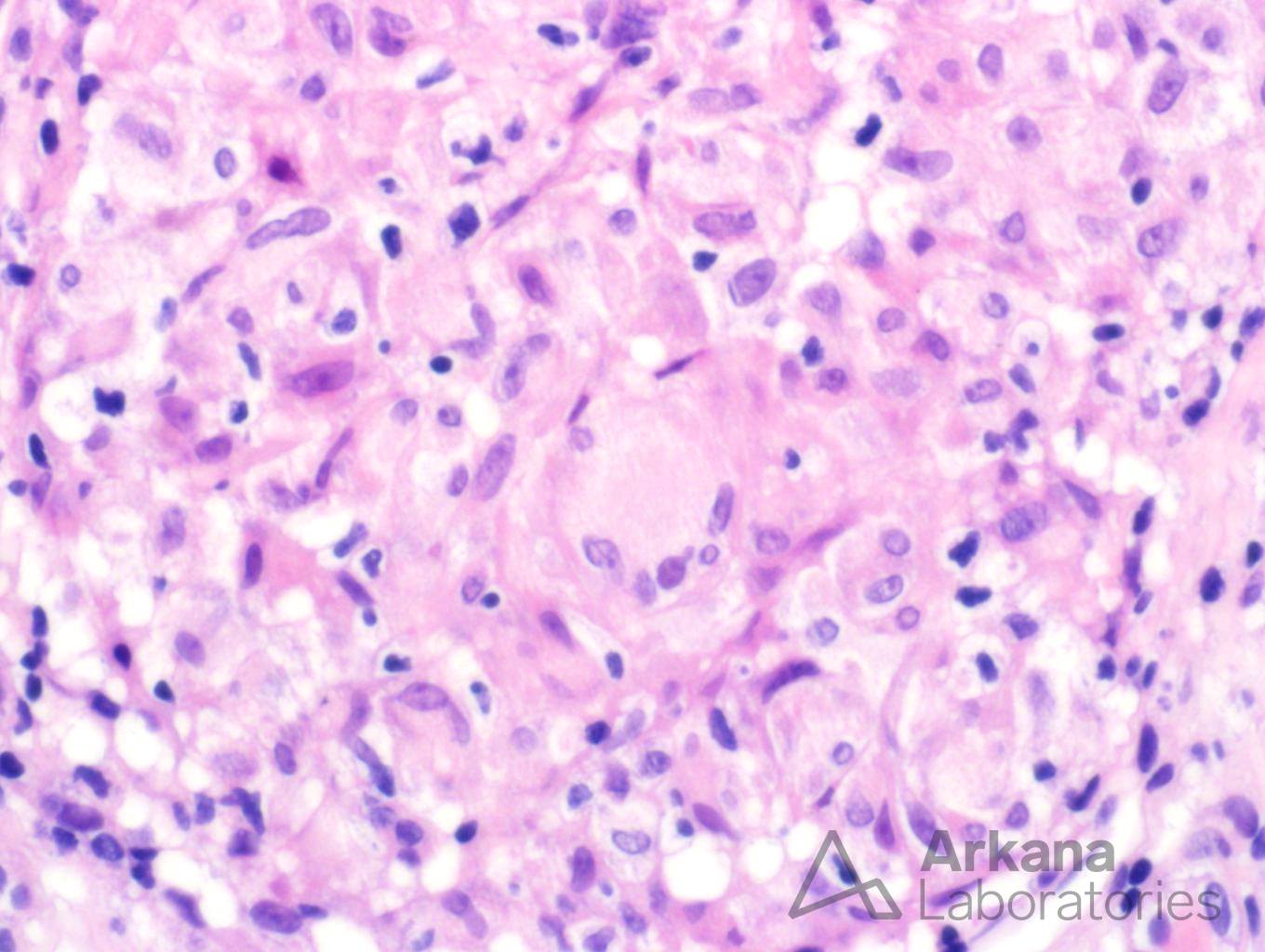
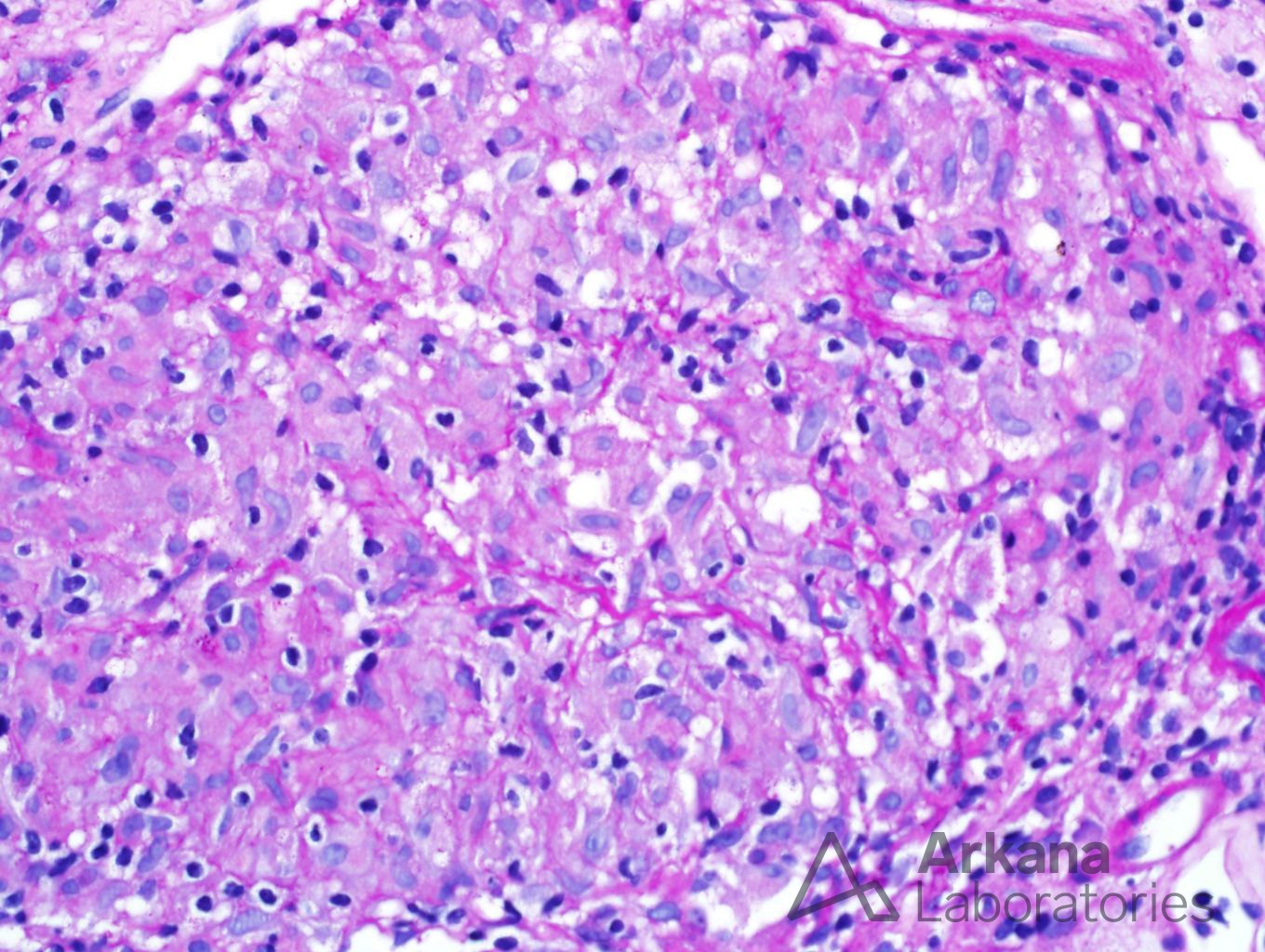
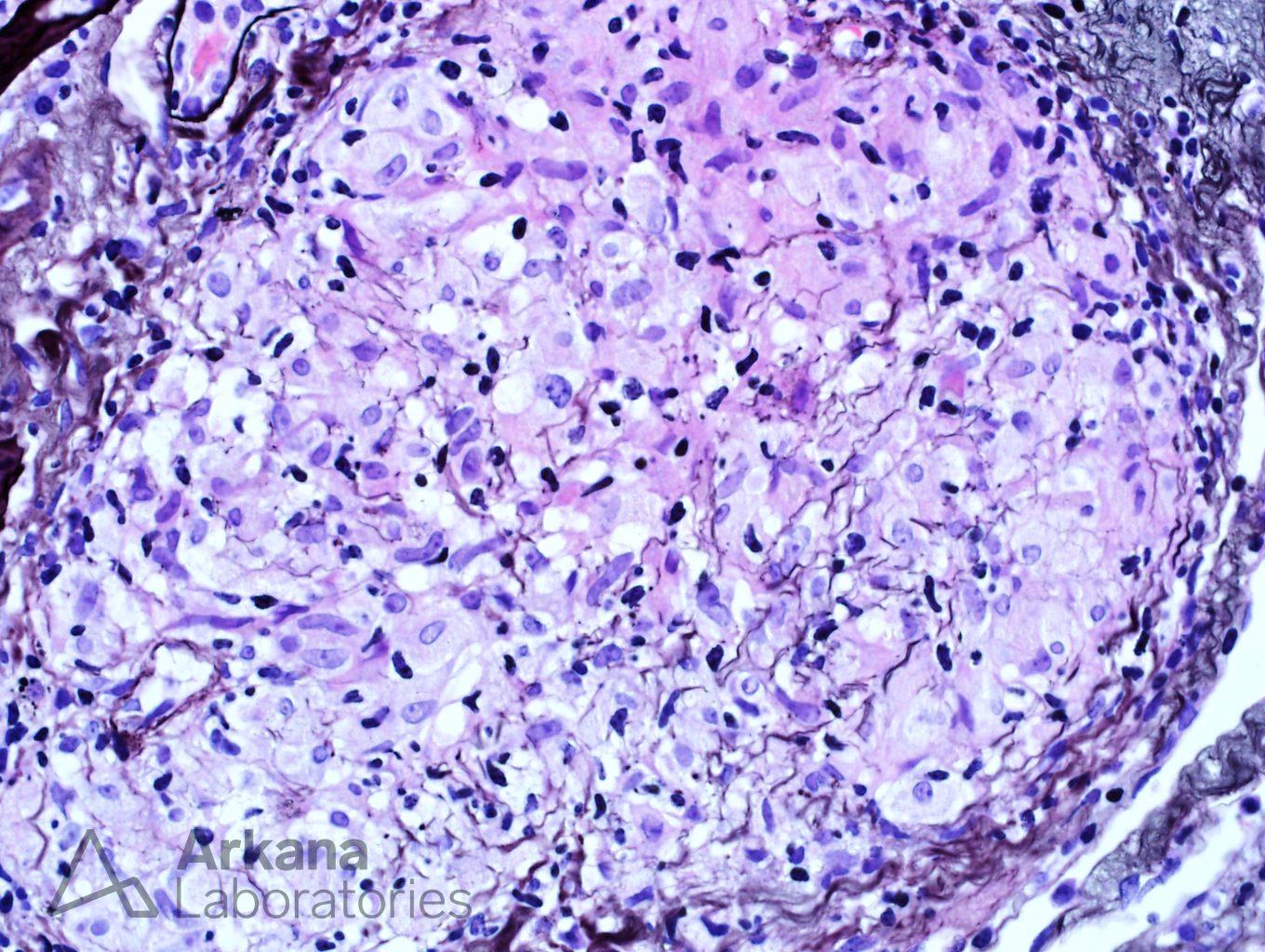
The biopsy shows a florid example of non-caseating granulomas throughout the interstitium. The granulomas are PAS and silver negative. Stains for mycobacteria (AFB) and fungus (GMS) are negative (not shown). Even though drug reactions are the most common cause of granulomatous interstitial nephritis, the presence of enlarged peribronchial lymph nodes and increased ACE level makes sarcoidosis a more likely etiology. One of the most difficult aspects of this case was determining if the granulomas were surrounding vasculature. In necrotizing vasculitis, giant cells and fibrinoid necrosis can be seen in and around vasculature. However, the lack of necrosis and overall distribution of granulomas within the interstitium helps rule out this potential etiology.
Quick note: This post is to be used for informational purposes only and does not constitute medical or health advice. Each person should consult their own doctor with respect to matters referenced. Arkana Laboratories assumes no liability for actions taken in reliance upon the information contained herein.